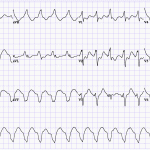
- Wide complex tachycardia is defined as a rate of > 100 with QRS > 120ms.
- Wide QRS represents slow activation of the ventricles that does not use the rapid His-Purkinje system of the heart.
- There are 5 classic causes of wide complex tachycardia mechanisms:
CLASSIC CAUSES OF WIDE COMPLEX TACHYCARDIA - Ventricular Tachycardia
- SVT with aberrancy (usually SVT with RBBB or LBBB)
- Pre-Excitation
- Pacing
- Artifact
(Another commonly cited cause is massive ST elevation)
- We encourage learners to state the above differential when asked to interpret a tracing with WCT.
- Remember: that a large majority of WCT is VT, especially if the patient has ischemic heart disease. WCTs should be treated as VT unless proven otherwise.
Basics
- Wide QRS complex suggests ventricular activation by:
- Impulse originating outside the normal conduction system, below the level of the AV node
- Impulse conducted down an abnormal His-Purkinje system (HPS) – aka aberrancy
- Pre-excitation with anterogradely conducted impulse over a bypast tract (BT)
Diagnostic Maneuvers
- Only should be done for hemodynamically unstable patients with crash cart ready to deliver cardioversion if necessary.
- Vagal maneuvers – can produce transient AV block, which can terminate some re-entrant SVTs.
- Adenosine
- Very helpful diagnostically to distinguish VT from SVT.
- Adenosine will result in a transient AV block, which may terminate some re-entrant SVTs, or block conduction to the ventricles to reveal atrial activity (such as atrial tachycardia).
- Adenosine generally has no effect on VT.
- Start with 6mg adenosine IV followed by rapid IV saline flush. If no effect, dose is doubled to 12mg IV. If no effect, then can be doubled to 24mg IV.
- With each injection warn the patient about the sensation of adenosine, and check to ensure the IV line is functional.
- No response to 24mg of adenosine generally means the tachycardia is insensitive to adenosine, and does not require the AV node in its mechanism (VT).
- NOTE: Some VT rhythms are adenosine sensitive, particularly outflow tract idiopathic VT.
Principles for distinguishing VT from SVT
- Two most important differential diagnoses of WCT are VT and SVT with aberrancy. Other differential diagnoses are often easily excluded:
- Pacing is easily ruled out with clinical history, physical exam, and absence of pacing spikes.
- Artifact can also be ruled out, as it often produces non-physiologic signals on ECG, often in a single lead.
- Pre-excitation (pre-excited SVT) is quite rare. The best tool is to look at the baseline ECG for evidence of pre-excitation.
- There are numerous scoring systems and algorithms developed to distinguish these two entities. (Brugada criteria, Vereckei algorithm, Lead II criteria, etc..). All of these algorithms are derived from the core principles, which we teach here. We recommend you become familiar with the Brugada criteria, since it is well known and frequently tested on exams.
- A useful approach is to start with a presumed diagnosis of VT, which will be correct 80-90% of the time. Significant proof is needed to dissuade you towards SVT.
- There are two main tools to distinguish VT from SVT with aberrancy: P-waves (AV dissociation) and QRS morphology – “how likely is it that this is an SVT with a bundle branch block?”
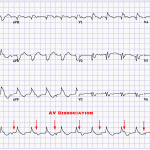
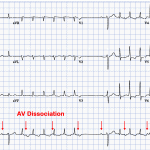
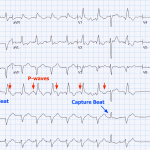
Principle #1: AV dissociation proves VT
- Highly favours VT (Spec 98%, Sens 82%), but only seen in 20-50% of VTs (Brugada et al 1992)
- AV dissociation proves that atria and ventricles are independently activated.
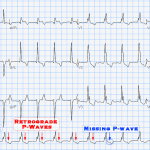
- A variation of this includes AV association but finding more QRSs than P-waves (see example). This proves that atria are not needed for the mechanism of the arrhythmia.
- Inability to find P-waves, or finding a 1:1 association between QRSs and P-waves is not helpful as both SVT and VT can produce this. About 30% of VTs conduct retrogradely to the atria, and have a 1:1 VA relationship. Whether the diagnosis is SVT (atria driving the ventricles) or VT (ventricles driving the atria) cannot be determined with a 1:1 AV relationship.
- TIP: Look for P-waves in leads with the smallest QRS. Best leads are II, V1, V2, I, and III.
- Advanced Tip: Look for wobble in the cycle length to see whether A or V move first. If the P-wave moves, and QRS follows, then atria are leading the ventricles, and VT can be excluded.
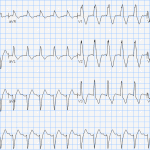
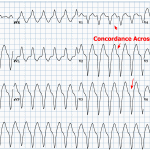
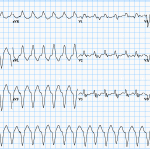
Principle #2: Concordance proves VT
- If all precordial leads demonstrate positive R-waves with no negative components, then VT is diagnosed. Similarly if all precordial leads are negative (QS waves) with no positive component, VT is diagnosed.
- This is the most specific criterion (Sp 100%, Sn 21%), but is rarely seen.
- The word “SVT with aberrancy” represents SVT that conducts down the ventricles with abnormal conduction – mostly bundle branch / fascicular blocks. This rule exists because there is no variation of LBBB or RBBB that can produce this pattern, hence VT is highly likely.
Principle #3: QRS is completely identical to the sinus QRS highly suggests SVT.
- Baseline ECG often establishes baseline conduction abnormalities
- WCT that has an identical QRS to sinus rhythm suggests that the ventricles are being activated in an identical way to sinus rhythm, which is most commonly SVT.
- This does not absolutely rule out VT due to the following exceptions:
- Septal VT with early access to the His-Purkinje system.
- Bundle branch reentrant (BBR) VT and interfascicular reentrant VT can produce a QRS with classic LBBB/RBBB, but they are rare and only seen in patients with dilated ventricles and severe LV dysfunction.
Principle #4: QRS with right superior axis (aka “extreme right axis” or “northwest axis”) is highly indicative of VT.
- There is no combination of bundle branch block or fascicular block that can produce this axis change.
- Initial positive force in aVR also suggests highly unusual initial activation of the ventricles.
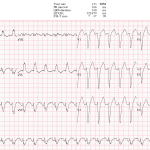
In absence of above principles, use QRS Morphology Criteria
- In absence of above findings, we end up with QRS morphology criteria asking the most basic question: How likely is this QRS morphology to represent LBBB or RBBB (+/- fascicular block)?
- Note that QRS morphology is probabilistic, and is diagnostically weaker because:
- It relies on the learner’s ability to identify a “typical” aberrancy pattern on a 12-lead ECG (BBB or fascicular blocks). We often suggest learners draw each lead of typical BBBs on blank paper.
- Highly unusual aberrancy patterns are frequently encountered. We have also seen VT morphology highly resembling BBB.
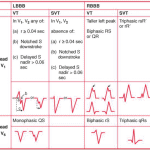
- Numerous studies have assessed aberrancy patterns (LBBB and RBBB-type), and found features that are “typical” and “atypical” for a BBB, associated with sensitivity/specificity for each. Brugada published many of those studies, and created an algorithm named “Brugada Criteria”. These features include:
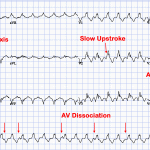
- LBBB and RBBB generally have rapid onset, representing conduction down the functioning bundle. Slow onset of QRS favours VT.
- Brugada demonstrated R-S time of 100ms as a cutoff (measured beginning of R to the nadir of the S in V1-V2).
- In cases of RBBB-type morphology (positive terminal QRS in V1)
- RBBB has rSR’ morphology –> the first r is never larger in amplitude compared to R’. If it is, suspect VT.
- RBBB should have a large positive component (R), and a small negative component (S) in V6. Absence of an R in V6, or an R that is smaller than S in V6 is unusual for an RBBB, and suggests VT.
- RBBB QRS duration is typically < 140ms, anything longer suggests VT.
- NOTE: This is a soft criteria, since many VTs are narrow and many BBBs are wide.
- In cases of LBBB-type morphology (negative terminal QRS in V1)
- LBBB generally has a negative component in V1. Downstroke of the S wave in V1 is smooth, and presence of notching on the downstroke suggests VT.
- LBBB QRS duration is typically < 160ms, anything longer suggests VT (very soft criteria).
- LBBB and RBBB generally have rapid onset, representing conduction down the functioning bundle. Slow onset of QRS favours VT.
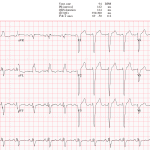
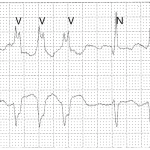
Fusion and Capture beats:
- Fusion beats: Simultaneous activation of ventricle by supraventricular impulse and ventricular beat resulting in intermediate QRS morphology
- Capture beats: QRS complex identical to underlying sinus rhythm occurs during the WCT – intermittent “capture” of ventricular activation by the normal conduction system
- Capture of fusion beats are rare, and suggest a diagnosis of VT. However, VT often can fuse with ventricular ectopy creating the appearance of capture and fusion beats.
- NOTE: Capture and fusion beats are important to understand because they frequently show up on exams.
Well Known Aberrancy (Ashman)
- Ashman phenomenon is an aberrant ventricular conduction due to change in QRS cycle length, and can be seen in supraventricular arrhythmias – commonly atrial fibrillation.
- This commonly produces an RBBB-type aberrancy, and is caused by a difference in relative refractory periods of the left and right bundles. Usually the right bundle branch has a longer refractory period than the left bundle branch, and takes longer to recover. When long R-R interval is followed by a shorter R-R interval timed such that the right bundle has not had adequate time to recover. These long-short sequences are followed by an RBBB-type morphology.
- Note for advanced learners: Usually aberrancy pattern is seen for several QRS complexes in a row. This is caused by transseptal conduction. The stimulus blocks in the RBB, and travels down the functioning LBB, then crosses the septum and retroconducts up the right bundle, which is now recovered. The next stimulus still finds RBB refractory because it was activated much later than the LBB, and has not had time to recover. This continues until there is a pause long enough for both bundle branches to recover.
- This type of aberrancy is commonly seen in patients with atrial fibrillation, and is often mistaken for VT.
Algorithms
- There are many well-validated algorithms to distinguish VT from SVT. However, we frown upon blindly memorizing algorithms because they are easy to forget, can be tricky to apply, and carry numerous pitfalls that are often forgotten.
- All algorithms are based on the principles we laid out above. We feel that understanding the pathophysiologic explanation for each principle will will establish a more durable and valuable skill set compared to memorizing an algorithm.
- However, algorithms are often frequently discussed by physicians, and are often found on exams. The most popular one is the Brugada Criteria. As an exercise, identify the above principles as steps in this brugada criteria:
- Step 1: Absence of RS complex in precordial leads (concordance)
- YES –> VT
- NO –> Go to Step 2
- Step 2: R to S interval >100msec in at least 1 precordial lead (slow activation)
- YES –> VT
- NO –> Go to Step 3
- Step 3: AV dissociation present
- YES –> VT
- NO –> Go to Step 4
- Step 4: Morphology criteria (above) for VT present in leads V1-V2 AND V6 (see table)
- YES –> VT
- NO –> SVT
- Other algorithms: (1) Bayesian, (2) Vereckei, (3) Griffith, (4) aVR, (5) Lead II R-waves Peak Time.
Further Reading
- 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death
- 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society Position Statement on the Management of Ventricular Tachycardia and Fibrillation in Patients With Structural Heart Disease
- Issa, Z. F., Miller, J. M., & Zipes, D. P. (2019). Clinical Arrhythmology and Electrophysiology. Philadelphia, PA: Elsevier.
Authors
- Primary Author: Dr. Pavel Antiperovitch (MD, FRCPC, EP Fellow), Dr. Yehia Fanous
- Author/Reviewer: pending
- Staff Reviewer: pending
- Copy Editor: pending
- Last Updated: Dec 14, 2020
- Comments or questions please email feedback@cardioguide.ca