Introduction
- Pulmonary Artery Catheters (PAC) also know as Swan-Ganz catheters are an advanced hemodynamic tool to evaluate a wide range of conditions.
- Though they used to be common place in many ICU’s, evidence suggesting lack of benefit in indiscriminate use has resulted in them falling out of favour.
- There is still a role in management of complex and critically ill patients.
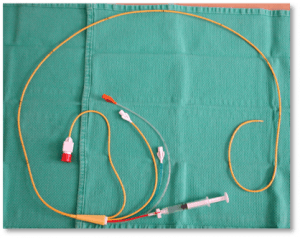
Insertion
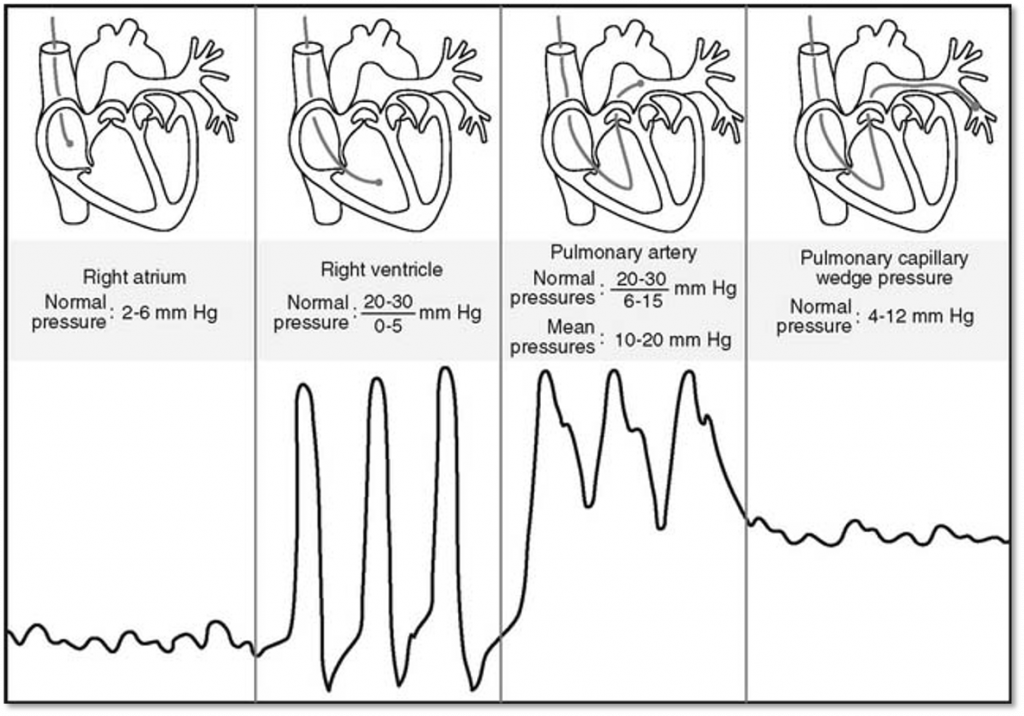
- Inserted typically in the right internal jugular and advance into the right atrium, right ventricle, pulmonary artery (PA) and left in the PA. It can be further advanced until it compresses a small pulmonary artery and the pressure measued as the pulmonary capillary wedge pressure [PCWP] (A surrogate for left atrial pressures).
Physiologic Measurements Provided
Direct Measurements
- Resting Hemodynamics
- Central Venous Pressure (CVP)
- Right atrial pressure (RAP)
- Right ventricular pressure (RVP)
- Pulmonary artery pressure (PAP)
- Pulmonary capillary wedge pressure (PCWP)
- Provides an estimate of left atrial pressure.
- Cardiac Output (CO) Thermodilution (see below)
- True mixed venous saturation. Mv02.
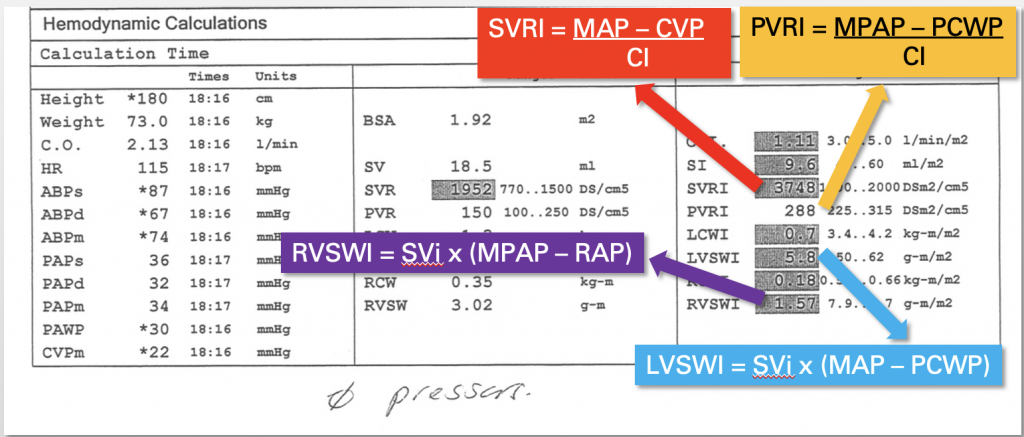
Indirect Measurements
A number of calculations can be achieved with the Swan providing additional hemodynamic data of the patient.
- Systemic Vascular Resistance = [MA(mean arterial pressure) – CVP/CO] x 80 (reported in Dynes units)
- Pulmonary Vascular Resistance = Mean PA – PCWP/CO (reported in Woods Units)
- Cardiac Index (CI) = CO/BSA (body surface area)
- Stroke Volume Index = CI/ HR
- Fick CO Calculation = 1.36 x hemoglobin x [Arterial sat – Mv02] (see below)
- Left Ventricular Stroke Work Index [LVSWI] = [MAP – PCWP] x SVi x 0.136
- Right Ventricular Stroke Work Index [RVSWI] = [Mean PAP – CVP] x SVi x 0.136
Note: The difference between Dynes and Woods units is a multiple of 80. Woods x 80 = dynes
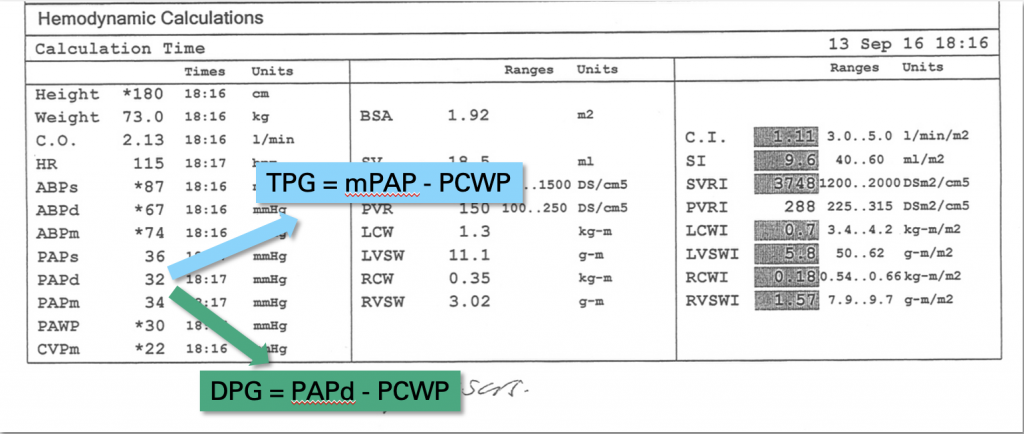
Other Important Calculations
- Diastolic Pulmonary Gradient (DPG) = (Diastolic Pulmonary Pressure – PWCP)
- Normal DPG < 7 (Suggests Isolated Post-capillary pulmonary HTN [Left Heart Failure])
- If 7 or greater suggest post-capillary and pre-capillary pulmonary HTN)
- Transpulmonary gradient = (Mean PAP – PWCP)
- Normal < 12
- If elevated suggest mixed pulmonary HTN.
- Right Atrial Pressure/ Pulmonary Capillary Wedge Pressure (RAP/PCWP)
- Can be helpful to assess for RV failure.
- Can be helpful a marker of biventricular failure and the degree of RV vs LV failure is involved. The greater the value the more the RV is involved in the problem.
- Elevated ratio suggestive of increase death, hospitalization, renal failure, RV failure after LVAD, and can be predictive of RV failure post-MI.
- Ratio > 0.63 suggestive of RV failure post-LVAD
- Ratio > 0.86 suggestive of RV failure post- myocardial infarction
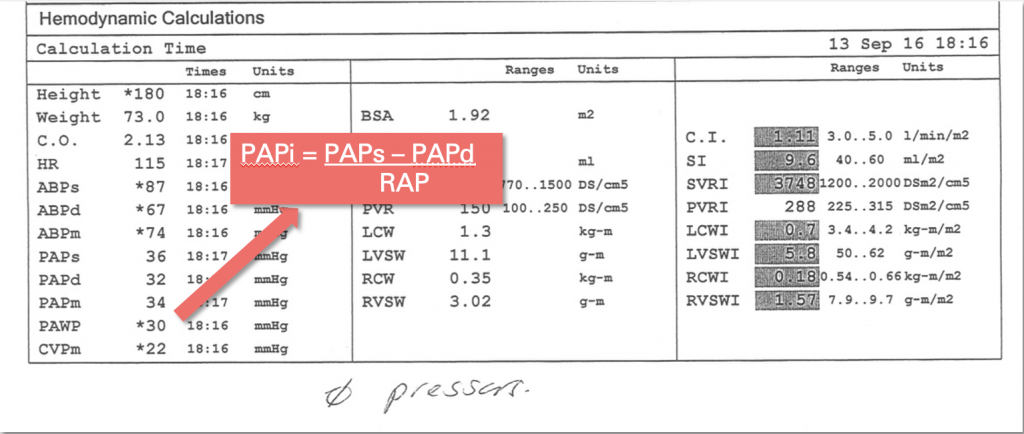
- Pulmonary Artery Pulsatility Index (PAPi) [(SPAP – DPAP)/RAP]
- Can be helpful to assess for RV failure.
- PAPi < 1.85 preditive of RV failure post- LVAD.
- PAPi < 1.0 predictive of RV failure post- myocardial infarction.
Cardiac Output Calculations
- Two Methods for determining cardiac output with a PAC Thermodilution and Fick.
- Thermodilution most commonly used in critical care settings since calculated with the PAC data.
- Fick Cardiac output involves using the mixed venous blood gas, hemoglobin, and math.
- Both have advantages and disadvantages.
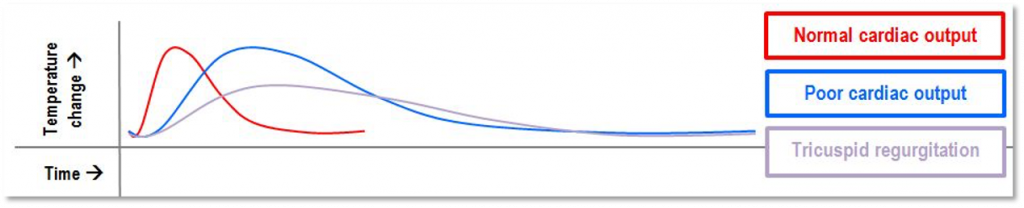
Thermodilution
- Known amount/temperature of saline injected into proximal port (RA) >> mixes and cools blood >> recorded by thermistor at distal end of catheter.
- Thermistor = a variable resistor, where resistance is proportional to temperature
- CO inversely proportional to AUC (temperature-time curve)
- Unreliable with:
- Intracardiac shunts (overestimates)
- Severe TR (underestimates)
- Severe PR (underestimates)
- Atrial fibrillation
- Severe LV dysfunction
Fick Cardiac Output
- AV difference = difference in oxygen content across the pulmonary circulation
- Oxygen content = blood O2 saturation x [Hb] x amount of O2 carried per gram of Hb
- Where: amount of O2 carried = 1.36mLO2/gHb x 10 >> to convert units (g/dL –> g/L)
- Oxygen consumption = rate at which O2 taken up by blood from lungs
- Historically measured by Douglas bag
- Now estimated (or “assumed Fick”)
- Normal = 125 mL/min/m2 (or 250mL/min for average BSA)
- Very elderly = 110 mL/min/m2
- Therefore:
- Fick CO Calculation = O2 consumption (ml/min) / A-V O2 difference
- Fick CO Calculation = 125 x BSA / 1.36 x hemoglobin x [Arterial Sats- Mv02]
- Less accurate in high output states (eg. Sepsis, hyperthyroid, cachexia), shunt.
Indications
- Unexplained Shock
- Severe Cardiogenic Shock
- Suspected or known Pulmonary Hypertension
- Decisions on Mechanical Support (MCS)
- Management of hemodynamic instability following cardiac surgery.
Note: Not an exhaustive list but common indications in coronary care units and cardiac ICU’s.
Contraindications
- Presence of left bundle branch block (LBBB) – Risk causing a RBBB with PAC insertion -> lead to complete heart block.
- Right sided lesions (cardiac tumour, thrombus, endocarditis) -> risk of embolizing into the PA.
- Profound Acidemia pH <7.1 (relative) -> Higher risk or arrhythmia’s.
- Prosthetic tricuspid or pulmonic valve.
- Tricuspid regurgitation – > Very challenging to float into the PA with severe regurgitation.
Complications
- Related to central venous puncture
- Arterial puncture / dilation (1.9%)
- Hematoma
- AV fistula
- Pseudoaneurysm
- Thoracic duct injury
- Pneumothorax / hemothorax (0.5%)
- Air embolism
- Thrombosis
- Subclavian (1.9%), IJ (7.6%), femoral (22%)
- Related to insertion / manipulation of SG catheter & long term placement / use
- Arrhythmia (12.5 – 70%)
- Sustained ventricular arrhythmia (< 1%)
- Transient RBBB (5%)
- Mechanical (0.9%)
- Risk factor = enlarged RV
- Limit risk by limiting catheter length < 60cm
- PA rupture, RV perforation >> ”exceedingly rare”
- Infection (1-2%)
- Arrhythmia (12.5 – 70%)
- PA rupture
- Rare, but serious
- 0.03 – 0.2%
- In review of > 32, 000 patients
- All had hemoptysis
- 70% mortality
- Proposed risk factors
- Age > 60
- PH
- Improper balloon inflation
- Improper positioning
- Cardiopulmonary bypass
- Anti-coagulation
- PA rupture management
- Intubation
- High PEEP
- Ruptured side down (if known)
- Consider single lung isolation
- IR vs. OR
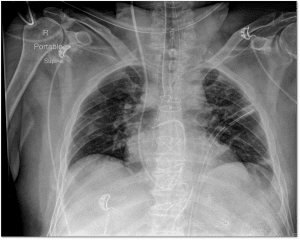
Chest X-ray position
Case examples
Case 1
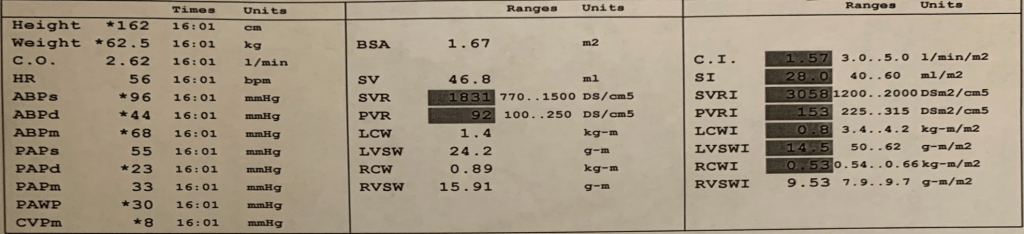
Resting Hemodyamics (Focus on left hand column):
- BP 96/44 mmHg. Mean BP 68 mmHg. Note a heart rate of 56 bpm
- Slightly elevated right atrial pressures.
- Pulmonary pressures 55/23 with a Mean of 33 mmHg -> Elevated pulmonary pressures with mild pulmonary hypertension.
- Elevated Wedge Pressure of 30 mmHg.
- Diastolic Pulmonary Gradient (DPG) = (Diastolic Pulmonary Pressure – PWCP) = 23 – 30 = -7
- (Suggests Isolated Post-capillary pulmonary HTN [Left Heart Failure])
- Transpulmonary gradient = (Mean PAP – PWCP) = 33 – 30 = 3
- Value of 3 suggest isolated post-capillary pulmonary HTN.
Cardiac Output and Vascular Resistance:
- Cardiac output (calculated by thermodilution) = 2.62 L/min (Normal 4 – 6)
- Cardiac Index 1.57 l/min/m2
- Low cardiac output and cardiac index.
- Elevated SVR 1831 dynes units (770-1500)
- Elevated SVRI 3058 (1200 – 2000)
- Patient vasoconstricted/ “clamped down”
- PVR 92 dynes. Traditionally reported in Woods Units. 92/80 = 1.15 WU
- Pulmonary vasoconstriction not an issue with this patient.
Conclusion:
- Isolated left heart failure.
- Normal right sided filling pressures.
- Mild Pulmonary HTN from left heart failure.
- Reduced cardiac output and cardiac index.
- Elevated systemic vascular resistance.
- Elevated left sided filling pressured (elevated wedge).
- Treatment considerations would include an ionodilator + diuresis: Increase cardiac output and decrease SVR. Examples dobutamine or milrinone. (Please see our module of cardiogenic shock)
Apical 4 chamber view showing isolated left heart failure consistent with swan interpretation.
Subcostal view showing isolated left heart failure consistent with swan interpretation.
Case 2
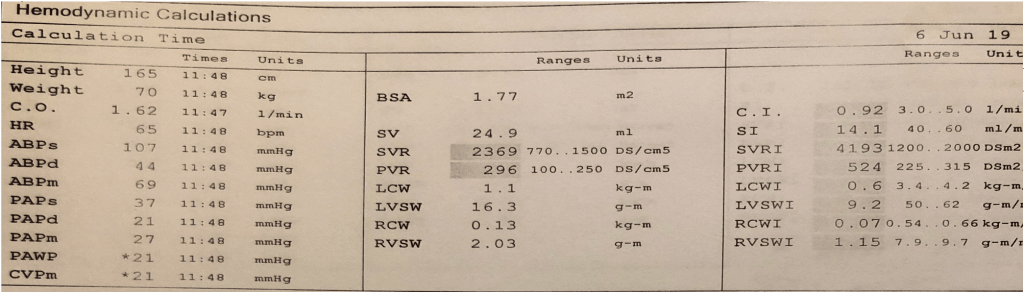
Resting Hemodyamics:
- BP 107/44 mmHg. Mean BP 69 mmHg. Note a heart rate of 65 bpm
- Right atrial pressures of 21 mmHg- > Severely elevated right sided filling pressures.
- Pulmonary pressures 37/21 with a Mean of 27 mmHg -> Elevated pulmonary pressures with mild pulmonary hypertension.
- Elevated Wedge Pressure of 21 mmHg.
- Diastolic Pulmonary Gradient (DPG) = (Diastolic Pulmonary Pressure – PWCP) = 21 – 21 = 0
- (Suggests Isolated Post-capillary pulmonary HTN)
- Transpulmonary gradient = (Mean PAP – PWCP) = 27 – 21 = 6
- Value of 6 suggest isolated post-capillary pulmonary HTN.
Cardiac Output and Vascular Resistance:
- Cardiac output (calculated by thermodilution) = 1.62 L/min
- Cardiac Index 0.92 l/min/m2
- Severely reduced cardiac output and cardiac index.
- Elevated SVR 2369 dynes units (770-1500)
- Elevated SVRI 4193 (1200 – 2000)
- Patient very vasoconstricted/ “clamped down”
- PVR 296 dynes. Traditionally reported in Woods Units. 296/80 = 3.7 WU
- There is pulmonary vasoconstriction
- In fact PVR > 3 WU suggest pulmonary HTN with a pre-capillary component. Despite the findings of our DPG.
Additional Calculations:
- Right Atrial Pressure/ Pulmonary Capillary Wedge Pressure (RAP/PCWP)
- Can be helpful to assess for RV failure.
- Can be helpful a marker of biventricular failure and the degree of RV vs LV failure is involved. The greater the value the more the RV is involved in the problem.
- Elevated ratio suggestive of increase death, hospitalization, renal failure, RV failure after LVAD, and can be predictive of RV failure post-MI.
- Ratio > 0.63 suggestive of RV failure post-LVAD
- Ratio > 0.86 suggestive of RV failure post- myocardial infarction
- In our case RAP/PCWP = 21/21 = 1 -> suggestive that RV failure is a major contributor to this case.
- Pulmonary Artery Pulsatility Index (PAPi) [(SPAP – DPAP)/RAP]
- Can be helpful to assess for RV failure.
- PAPi < 1.85 preditive of RV failure post- LVAD
- PAPi < 1.0 predictive of RV failure post- myocardial infacrtion
- In our case the PAPi [(SPAP – DPAP)/RAP] = 37 – 21/ 21 = 0.76
Conclusions:
- Biventricular failure RV > LV
- Significantly elevated right sided filling pressures
- Mild Pulmonary HTN possibly mixed pre/post capillary given discrepancies between PVR and DPG/TPG.
- Severely reduced cardiac output and cardiac index.
- Severely elevated systemic vascular resistance.
- Elevated left sided pressures (high wedge).
- Elevated PCWP suggests there is an element of LV failure.
- Elements of advanced RV failure PAPi + RAP/PCWP.
- Treatment considerations would include an ionodilator + diuresis: Increase cardiac output and decrease SVR. Examples dobutamine or milrinone. (Please see our module of cardiogenic shock)
Parasternal long axis view showing bi-ventricular failures consistent with the swan interpretation. Notice the pleural effusion and “hepatized” lung. There is also a trivial pericardial effusion. You can distinguish the two as pericardial fluid wraps anterior to the descending aorta. You can also visualize the swan in the RVOT on this view.
Apical 4 Chamber view showing bi-ventricular failure consistent with the swan interpretation. You can see in this view again the pleural effusion and “hepatized lung” on the lateral wall.
Case 3
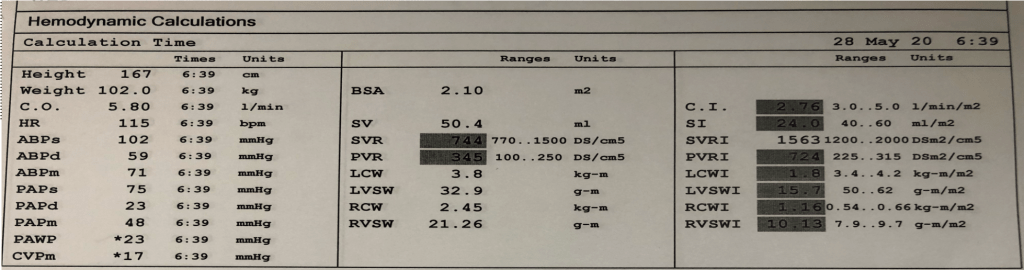
Resting Hemodyamics:
- BP 102/59 mmHg. Mean BP 71 mmHg. Note a heart rate of 115 bpm
- Right atrial pressures of 17 mmHg- > Severely elevated right sided filling pressures.
- Pulmonary pressures 75/23 with a Mean of 48 mmHg -> Severely elevated pulmonary pressures with severe pulmonary hypertension.
- Elevated Wedge Pressure of 23 mmHg.
- Diastolic Pulmonary Gradient (DPG) = (Diastolic Pulmonary Pressure – PWCP) = 23 – 23 = 0
- Note in this case the PWCP is likely not accurate here. Notice how the DPAP and PCWP are the same? A common practice in ICU’s with patients with Swan is not perform a capillary wedge pressure. Instead the DPAP is assumed to be the PCWP. This is generally true in patients with isolated group 2 (left heart failure) patients. But this assumption may not be correct in mixed cases or pre-capillary pulmonary HTN.
- Transpulmonary gradient = (Mean PAP – PWCP) = 48 – 23 = 25
- Value of 25 suggestive of pre-capillary pulmonary HTN.
Cardiac Output and Vascular Resistance:
- Cardiac output (calculated by thermodilution) = 5.8 L/min
- Cardiac Index 2.76 l/min/m2
- Mild reduction in cardiac output when indexed for BSA.
- Elevated SVR 744 dynes units (770-1500)
- Elevated SVRI 1563 (1200 – 2000)
- Patient has normal systemic vascular resistance.
- They are not “clamped down”
- PVR 345 dynes. Traditionally reported in Woods Units. 345/80 = 4.3 WU
- There is pulmonary vasoconstriction
- PVR > 3 WU suggest pulmonary HTN with a pre-capillary component.
Additional Calculations:
- Right Atrial Pressure/ Pulmonary Capillary Wedge Pressure (RAP/PCWP)
- In our case RAP/PCWP = 17/23 = 0.74 -> Possible RV failure.
- Pulmonary Artery Pulsatility Index (PAPi) [(SPAP – DPAP)/RAP]
- In our case the PAPi = 75 – 23/ 17 = 3.05
- Normal PAPi -> Suggest RV normal.
Conclusions:
- Severe pulmonary hypertension.
- Significantly elevated right sided filling pressures
- Severe pulmonary HTN with major pre-capillary component.
- Mildly reduced cardiac output when indexed.
- Normal systemic vascular resistance
- Elevated left sided pressures? Need to formally wedge. DPAP may not equal PCWP in this case.
- Treatment considerations would be pulmonary HTN related. An inhaled pulmonary dilator such as nitric oxide or epoprostenol can be considered for severe cases. A systemic pulmonary vasodilator such as milrinone could be used. Diuresis. Vasopressin the preferred vasopressor since won’t increase pulmonary vascular resistance. Consider expert opinion for pulmonary hypertension medications. (Please see our module of cardiogenic shock)
Off Axis 4 chamber with colour showing a severe dilated and failing right ventricle with tricuspid regurgitation consistent with RV failure and pulmonary hypertension.
Parasternal short axis showing a severe dilated right ventricle. Notice the D-shape of the left ventricle in systole and diastole consistent with right ventricle volume and pressure overload.
Case 4
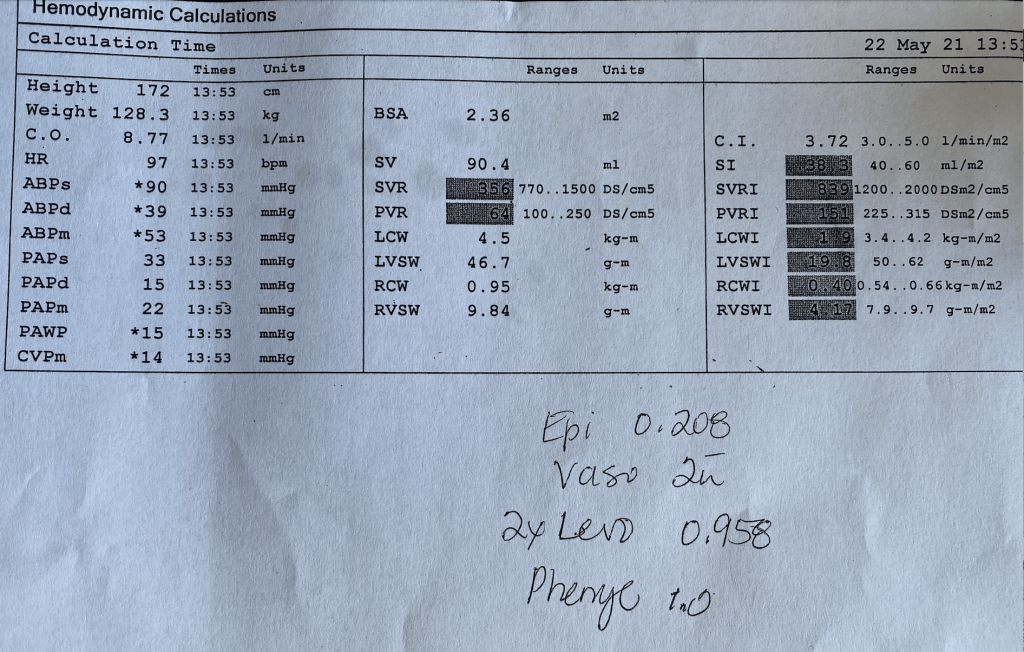
Resting Hemodyamics:
- BP 90/39 mmHg. Mean BP 53 mmHg. Note a heart rate of 97 bpm. This is on massive amounts of pressors (Epinephrine, Vaso, Norepinephrine, and Phenylephrine)!
- Right Atrial Pressure of 14mmHg.
- Pulmonary pressures of 33/23 with a mean of 22 mmHg -> No pulmonary HTN
- Wedge Pressure of 15 mmHg.
Cardiac Output and Vascular Resistance:
- Cardiac output (calculated by thermodilution) = 8.77 L/min
- Cardiac Index 3.72 l/min/m2
- This is not a cardiac output problem!
- Decreased SVR 356 dynes units (770-1500)
- Decreased SVRI 839 (1200 – 2000)
- Patient has severely reduced systemic vascular resistance and is on massive doses of pressors -> This is severe vasodilation/vasoplegia.
- PVR 64 dynes. Traditionally reported in Woods Units. 64/80 = 0.8 WU
- There is pulmonary vasodilation as well.
Conclusions:
- Severe vasodilatory shock! Severely reduced SVR/SVRI. Patient on massive doses or pressors and still vasodilated.
- Elevated cardiac output.
- Normal filling pressures.
- In cardiac ICU’s the two big considerations are post-pump vasoplegia or septic shock.
Parasternal short axis view showing hyperdynamic left ventricle consistent with distributive shock and the swan interpretation.
Further Reading
- Mechanical Circulatory Support Devices for Acute Right Ventricular Failure. American Heart Association. Navin Kapur et al. 2017.
- Relationship of Right- to Left-Sided Ventricular Filling Pressures in Advanced Heart Failure: Insights From the ESCAPE Trial. American Heart Association. Mark Drazner et al. 2013.
- Executive Summary of the SCAI/HFSA Clinical Expert Consensus Document on the Use of Invasive Hemodynamics for the Diagnosis and Management of Cardiovascular Disease. Journal of Cardiac Failure. Michael Givertz et al. 2017.
- Complications Associated With Pulmonary Artery Catheters: A Comprehensive Clinical Review. Scandinavian Journal of Surgery. D.C. Evans et al. 2009
Authors
- Authors: Dr. Daniel Durocher (MD, FRCPC, Cardiologist, ICU Fellow)
- Staff Reviewer: Dr. Faizan Amin (MD, FRCPC, Cardiologist, Intensivist])
- Last Updated: May 7, 2022