Introduction
- Required Reading: Introduction to Arrhythmia Diagnosis
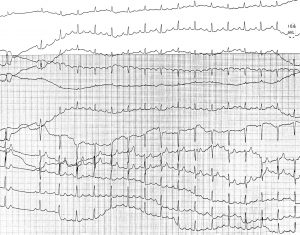
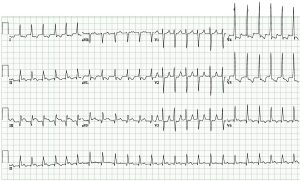
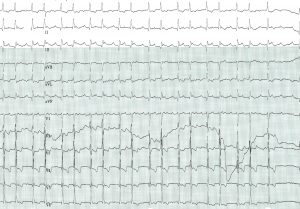
- Narrow QRS tachycardia can be split into two categories: regular (also known as SVT or supraventricular tachycardia) and irregular.
- It is important to use an approach when assessing a narrow QRS tachycardia: describe the ECG, present a differential diagnosis and then narrow the differential.
- Acute care of narrow QRS tachycardia is guided by the ACLS algorithm.
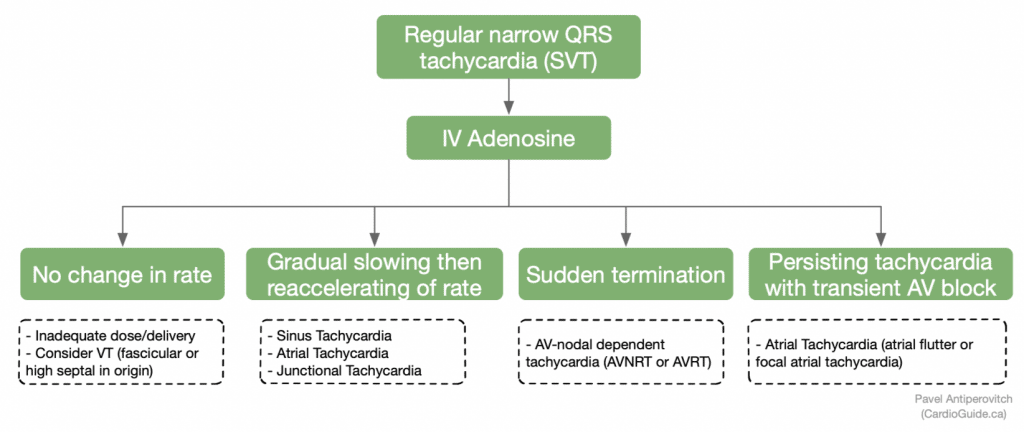
- In stable patients, adenosine is a very important tool in both treatment of certain SVTs and diagnosis.
- Chronic management is guided by diagnosis and patient symptoms. Patients can benefit from referral to a specialist as SVTs can be controlled with antiarrhythmics or procedures. Atrial fibrillation has its own important implications, ie. stroke prevention.
Background
- Narrow QRS tachycardia is defined as a tachycardia (heart rate >100) with narrow QRS (duration <120 ms).
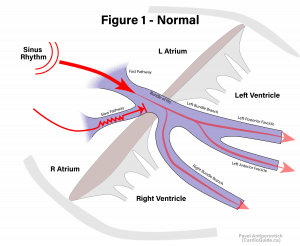
- Narrow QRS indicates simultaneous activation of both ventricles
- Atrial tachycardias generally have a narrow QRS because their ventricular activation occurs via the AV node and the ventricular conduction system (His-Purkinje system), which leads to simultaneous activation of both ventricles.
- NOTE: Atrial tachycardias can have a wide QRS, often in the presence of a RBBB, LBBB, or pre-excitation.
- NOTE: The term “SVT – Supraventricular Tachycardia” refers to narrow QRS REGULAR tachycardia. Even though atrial fibrillation is “supraventricular,” it is not classically called “SVT.”
The Approach
- Describe the ECG & frame the problem
- Step 1: Narrow vs. wide (≥120ms?)
- Step 2: Regular vs. irregular (use calipers)
- Present a differential diagnosis (see Tables)
- Narrow the differential diagnosis (understanding the mechanisms of arrhythmia)
| DDx of an IRREGULAR narrow QRS Tachycardia: |
NOTE: This list is not exhaustive; other mechanisms exist |
| Differential Diagnosis of a REGULAR Narrow QRS Tachycardia |
|
Approach to diagnosis
Medical students and PGY1-2 residents should make the distinction between irregular narrow complex tachycardia and regular narrow complex tachycardia (aka SVT), and should know the differential diagnosis and the initial management for each. Distinguishing between the types of SVTs is advanced, and is unlikely to make a difference in the acute and subacute management of the arrhythmia.
Advanced Diagnosis of SVT
(Recommended for PGY3 and above once you have the initial understanding and approach to arrhythmias)
Acute Management
Overall Approach
- Determine if STABLE vs. UNSTABLE
- Assess for hypotension, shock, altered LOC, new/worsening heart failure, ischemic chest pain.
- If the patient is unstable, the treatment is usually synchronized cardioversion.
- Determine if REGULAR vs. IRREGULAR because the management is slightly different.
- Breathe!
- A stable patient with a narrow QRS tachycardia is not a medical emergency.
- Take the time to fully assess the patient, and consider treatment options below.
- You often don’t need the tachycardia diagnosis to treat the patient acutely, so don’t get hung up on the ECG.
The most important thing is to follow the approach!
NOTE: The approach to a narrow QRS tachycardia is nicely summarized in the AHA ACLS Guideline (right side)
REGULAR Narrow Complex Tachycardia (SVT)
- Assess ABCs
- If patient is unstable (i.e. symptomatically hypotensive, or evidence of ischemia/shock): deliver SYNCHRONIZED cardioversion
- Vagal maneuvers (use in stable patient)
- Effectiveness: 19-54%
- Mechanism: stimulate carotid body to initiate parasympathetic response – this creates AV-nodal delay/block and terminates tachycardia.
- Valsalva maneuver (17% success): internationally recognized as first-line
- Modified Valsalva maneuver (43% success):
- Start semi-recumbent. After valsalva, change position to supine and raise legs.
- Blowing into a 10cc syringe can help ensure adequate valsalva
- Modified Valsalva infographic
- Video demonstration
- Carotid massage
- Auscultate to ensure no bruit. Do not perform if prior TIA/stroke.
- Extend neck, turn away from the side of interest. Apply constant pressure for no more than 5 seconds.
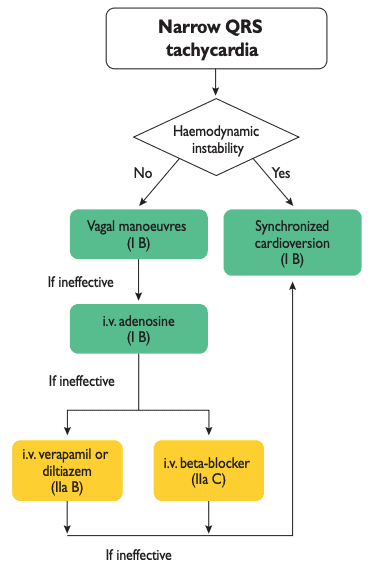
- Adenosine (See section below on adenosine)
- Beta blocker
- Contraindications: Hypotension and heart failure
- PO metoprolol 25-50 mg is most common: It is short-acting and titratable.
- IV beta blockers
- Metoprolol 2.5-15 mg IV in 2.5 mg boluses
- Esmolol (0.5 mg/kg bolus or 0.05-0.3 mg/kg/min infusion)
- Calcium channel blockers
- Contraindicated in:
- Hemodynamic instability (hypotension)
- Heart failure with reduced LVEF
- Suspicion of VT (can exacerbate hypotension)
- Pre-excited AF
- May be more effective than beta blockers at rate control, however they have additional side effects of exaggerated hypotension and negative inotropy, which can exacerbate heart failure.
- Diltiazem 20 mg over 2 minutes
- Verapamil 5-10 mg over 2 minutes
- NOTE: Oral medications are preferred for safety reasons. The only reason to use IV medications is if the patient is significantly symptomatic, and faster onset is preferred.
- Contraindicated in:
- Amiodarone
- Indications:
- Hemodynamically unstable + refractory to cardioversion
- Acute heart failure
- Amiodarone IV 150 mg boluses + (if needed 60 mg/hr IV infusion)
- Indications:
- Digoxin
- Option for patients with HF and AF
- 1 g load (0.5 mg IV + 0.25 IV x2 doses q4h)
IRREGULAR Narrow Complex Tachycardia
- Acute management is similar to REGULAR narrow complex tachycardia, with a few notable differences:
- Generally no role for vagal maneuvers
- Generally no role for adenosine
- (None of the irregular NCTs on the differential diagnosis require the AV node as part of their mechanism)
Adenosine
- Introduction:
- Can terminate AV-nodal dependent tachycardias (ones that require AV node as part of their mechanism)
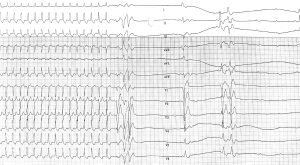
- If it does not terminate the tachycardia, the rhythm strip provides important diagnostic information (ALWAYS run a 12-lead continuous ECG strip)
- Indications:
- Hemodynamically stable narrow QRS regular tachycardia
- How to administer:
- Place the patient on cardiac monitoring (small case-report risk of AF and VF).
- Counsel the patient on sensation of adenosine (10-20 seconds of dyspnea and flushing).
- Connect a 12-lead ECG and ask the technologist to run CONTINUOUS 12-lead strip
- Deliver 6 mg IV bolus into a proximal IV (i.e. antecubital), followed by a quick flush (many physicians use a 3-way stopcock)
- Interpreting the result:
- Anticipated response: AV block or pause (even for one beat)
- If no effect, give 12 mg, and 18 mg if patient is agreeable.
- Adenosine slows the sinus rate and blocks the AV node via the A1 receptor.
- Tachycardias that terminate and convert to sinus rhythm are called “Adenosine-sensitive.”
- Adenosine-sensitive tachycardias are generally those that use the AV node as part of their circuit (AV nodal dependent). They are generally AVNRT and AVRT.
- NOTE: In rare cases, atrial tachycardia and flutter can terminate with adenosine. Just remember that “adenosine-sensitive” makes AVNRT/AVRT more likely, but does not rule out other mechanisms.
- P-waves can often be revealed, which helps determine the mechanism.
- Anticipated response: AV block or pause (even for one beat)
Chronic Management
Chronic management depends on the mechanism of the tachycardia.
NOTE: SVT is generally a benign condition with a good prognosis. Patients with infrequent, minimally symptomatic, self-limiting episodes may not need chronic therapy.
- Focal Atrial Tachycardia
- Ablation (Class 1): EP referral
- Medical Management
- Beta blocker / CCB / anti-arrhythmic (propafenone or flecainide)
- Ivabradine with beta-blocker can be considered
- Amiodarone
- Sinus Tachycardia
- Treat reversible causes
- Ivabradine or beta blocker can be considered in highly symptomatic cases.
- AVNRT
- Catheter ablation (Class 1): EP referral
- Minimally symptomatic/infrequent → may not need therapy
- Medical management
- Diltiazem or verapamil in patients without HFrEF
- Beta blockers
- AVRT
- Catheter ablation (Class 1): EP referral
- Medical management
- Orthodromic AVRT → Beta blocker or diltiazem/verapamil
- Antidromic AVRT → Propafenone/flecainide
- Atrial Fibrillation and Flutter
- Decide rate- vs. rhythm-control
- Anticoagulation for stroke prevention
- (See separate topic on atrial fibrillation)
Further Reading / References
- ESC 2018: Supraventricular Tachycardia Guidelines (HTML)
Special (Common) Cases
Narrow QRS Tachycardia and Hypotension
- Presents a challenge because using beta-blockers and calcium channel blockers is contraindicated in patients who are hypotensive.
- However, slowing down the rate is important because diastolic filling is reduced in tachycardias faster than > 150 bpm, and cardiac output would be reduced.
- You have 3 options:
- Electrical cardioversion – Generally requires sedation (unless patient is not conscious)
- Amiodarone IV – Generally neutral effect on blood pressure, generally acts as a B-blocker acutely (chronically it is an anti-arrhythmic)
- Digoxin IV – Neutral effect on blood pressure
Narrow QRS Tachycardia and Heart Failure
- It is often unclear if the mechanism of the heart failure is poor diastolic filling due to fast tachycardia (> 150 bpm), reduced LV systolic function due to chronic uncontrolled tachycardia (aka tachycardia-mediated cardiomyopathy), or LV dysfunction due to another cause which caused atrial fibrillation by increasing left atrial pressure.
- Beta blockers and calcium channel blockers are negative inotropes and are contraindicated in acute heart failure due to the risk of triggering worsening pulmonary edema and cardiogenic shock.
- 4 management options:
- Electrical cardioversion – Generally requires sedation, which is challenging because the patient is hypoxemic, and sedation can reduce their respiratory drive.
- Amiodarone IV – Very common agent that is generally safe in patients with heart failure.
- Digoxin IV – Provides mild positive inotropy, and can reduce the rate of the tachycardia (although the rate control effect is often very mild).
- **Diuresis** – (Most important) – Treating the patient’s heart failure can reduce sympathetic tone and left atrial pressure, which often drive atrial and ventricular tachycardias.
- Practical tip – If the patient will be managed in a monitored unit, amiodarone and diuretics are used. If the patient is on the ward, digoxin and IV diuresis may be enough for acute management. It is not always necessary to establish rate control as soon as possible.
- It may be acceptable to avoid overly aggressive initial rate-control, and initiate IV diuretics, which will improve the patient’s rate over time by treating their heart failure.
Contributors
- Primary Author: Dr. Pavel Antiperovitch MD, FRCPC, EP Fellow)
- Author/Reviewer: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Staff Reviewer: pending (MD, FRCPC[Cardiology])
- Copy Editor: Perri Deacon (medical student)
- Last Updated: Aug 20, 2020
- Comments or questions please email feedback@cardioguide.ca