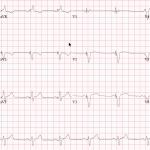
- Important to rapidly recognize patients with an acute STEMI as time matters in saving myocardium and lives.
- Clinicians need to be vigilant in recognizing ECG’s and know when to consider thrombolysis.
- When available percutaneous coronary intervention (PCI) is preferred to thrombolysis.
- Randomized trials have consistently shown better outcomes in terms or mortality and ischemic events with PCI.
- Major complications such as intracranial hemorrhage are reduced with PCI.
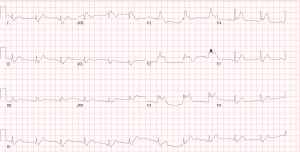
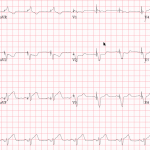
Case 1
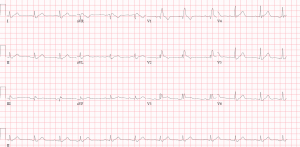
Case 2
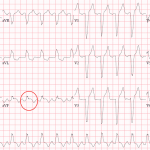
Sgarbossa Criteria
- Left Bundle Branch Blocks (LBBB) are uniquely challenging at interpreting for ischemic changes as ST changes are frequently seen in with LBBB that may or may not be related to ischemia.
- LBBB are always considered pathological but are not always associated with a myocardial infarction. Decisions regarding thrombolysis and cath lab activation can be difficult.
- Sgarbossa criteria first described by Elena Sgarbossa offers another tool for assessing for ischemic changes in the context of a LBBB or ventricular paced rhythm.
Criteria
- Concordant ST-Elevation of 1 or more mm = 5 points
- Concordant ST-depression of 1 or more mm in V1-V3 = 3 points
- Discordant ST-elevation of more that 5 mm = 2 points
Score of 3 or more has a 90% specificity for myocardial infarction. Not sensitive.
NOTE: For those who don’t like memorization, check every lead for the “Rule of LBBB”: In a LBBB the ST segment and T-wave always shift in the opposite direction of the main QRS vector (aka “discordant”). In a patient with acute chest pain, if this rule is broken, suspect a STEMI. The only exception is V1-V3, where QRS is always negative in a LBBB, in that case we look for excessive discordance (ST elevation of > 5mm).
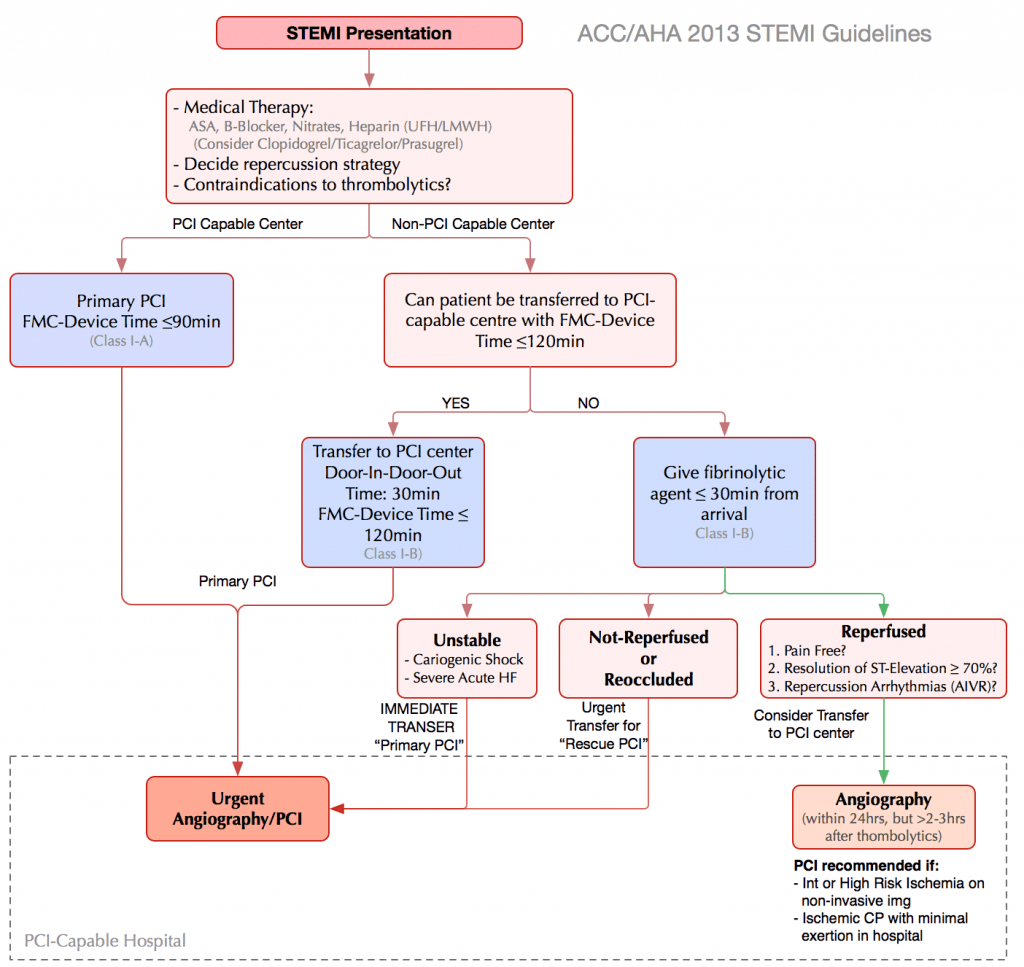
Thrombolysis in STEMI
When to Ship/When to Drip
- If high-quality primary PCI can be delivered within 120 minutes of first medical contact it is preferred to fibrinolytic therapy for most patients with STEMI.
- Ideally, PCI should be performed within 90 minutes from the time of first medical contact.
- If thrombolysis is planned it should be delivered within 30 minutes of hospital arrival
When to Thrombolyse
- No Contraindications!
- Patients with chest pain suggestive of acute myocardial ischemia who present up to 12 (possibly up to 24 hours) after symptom onset of symptoms are candidates for reperfusion with fibrinolytic therapy.
- The magnitude of the reduction in the risk of death in randomized trials is generally between 15 and 30 percent.
- The benefit from fibrinolytic therapy declines rapidly as the time from onset of symptoms grows.
Absolute Contraindications
- Any history of intracranial hemorrhage.
- Ischemic stroke within 3 months.
- Intracranial neoplasm or structural cerebral vascular lesion (exp. arteriovenous malformation).
- Suspected aortic dissection. (Occasionally dissection with present as inferior STEMI)
- Active internal bleeding.
- Closed head/face trauma in last 3 months.
Relative Contraindications
- Severe hypertension of sBP > 180 mmHg, or dBP > 110 mmHg.
- Any history of ischemic stroke.
- Major trauma in past 2-4 weeks.
- Non-compressible vascular puncture.
- Pregnancy.
- Active peptic ulcer.
- Use of anticoagulants.
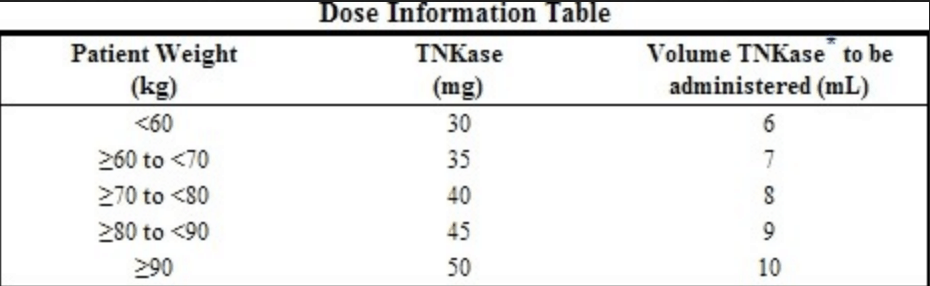
Tenecteplase (TNK) is the Thrombolytic of Choice
- Multiple thrombolytics available on the market.
- TNK is used for STEMI patients because of the ASSENT II Trial.
- This trial compared TNK to TPA.
- No difference in mortality.
- ICH was 1% in both groups.
- There was a significant reduction in non-cerebral and need for blood transfusions.
Adjunctive Therapies
- ASA load (162 mg) -> Then 81 mg for life.
- Clopidogrel load (300 mg) then 75 mg daily. Generally don’t load patients over the age of 75.
- Do not give Ticagrelor or Prasugrel when thrombolysis planned.
- Anticoagulation (Three Options).
- Heparin: 60units/kg bolus (Max 4000 units) followed by 12mg/hour infusion titrate to protocol. PTT 50-70. Note the Max dose is lower for thrombolysis vs PCI (Max 5000 units).
Enoxaparin: Age <75 years use a loading dose of 30 mg IV bolus followed by 1 mg/kg subcutaneously every 12 hours (maximum of 100 mg for the first two doses only).
In patients ≥75 years no loading dose and 0.75 mg/kg subcutaneously every 12 hours (maximum of 75 mg for the first two doses only).
- Fondaparinux: giving 2.5 mg intravenously, followed by 2.5 mg subcutaneously once daily.
- High Dose Statin: Atorvastatin 80mg daily or Rosuvastatin 40mg daily.
- Beta-Blocker: Contraindicated is active heart failure or shock or hemodynamic concerns.
- ACE-Inhibitors: Should be started within 24 hours.
Failed Lysis (Transfer Immediately for Rescue PCI)
- Persistent or worsening chest pain
- Persistent or worsening ST segment elevation -> looking for a 50% reduction in ST segment at 90 minutes.
- Hemodynamic instability or heart failure.
Clinical Pearls
- Do not wait for biomarkers -> Thrombolyse on clinical presentation and EKG.
- Clopidogrel is the antiplatelet of choice when the decision is made to thrombolyse.
- If PCI can be performed within 120 minutes of first medical contact this is the preferred treatment.
- May not be sufficient benefit to thrombolyse after 12 hours especially is no ongoing symptoms of chest pain (completed infarct) discuss with cardiology!