Abbreviations
- MR – Mitral Regurgitation
- LV – Left Ventricle
- MVP – Mitral Valve Prolapse
- POCUS – Point Of Care Ultrasound
- HOCM – Hypertrophic Obstructive Cardiomyopathy
- TTE – Transthoracic Echocardiography
- TEE – Trans-esophageal Echocardiography
- LBBB – Left Bundle Branch Block
- CRT – Cardiac Resynchronization Therapy
Introduction
- Mitral regurgitation (MR) can be categorized into acute vs. chronic.
- Acute: Sudden onset mitral regurgitation, often causing severe hemodynamic instability requiring urgent valve surgery
- Acute MR is a surgical emergency
- Chronic: primary vs. secondary MR
- Primary Chronic Mitral Regurgitation (Degenerative)
- Mitral valve disease involving the valve leaflets or subvalvular apparatus
- Examples include: mitral valve prolapse (MVP), rheumatic heart disease, endocarditis, severe valve calcification, Marfan Syndrome or Ehlers-Danlos Syndrome affecting leaflets
- Primary MR can be treated surgically with primary valve repair or replacement
- Secondary Chronic Mitral Regurgitation (Functional)
- “Secondary” to LV dilation causing annular dilation, which results in malcoaptation of mitral valve leaflets (i.e. the leaflets cannot reach each other during closure, which creates a central orifice)
- Usually treated non-surgically with medical therapy meant to reduce LV/annular dilation. Some intervention options available if medical therapy has failed (see below)
- Primary Chronic Mitral Regurgitation (Degenerative)
- Acute: Sudden onset mitral regurgitation, often causing severe hemodynamic instability requiring urgent valve surgery
- It is critical to identify the cause of mitral regurgitation because it directs management
- Good echocardiography reports will suggest a cause if MR is severe
Acute Mitral Regurgitation
- Acute MR is a life threatening disease that causes acute pressure and volume overload of the left atrium and ventricle leading to pulmonary congestion and poor cardiac output
- Causes:
- Leaflet disruption/rupture/perforation (i.e. endocarditis)
- Papillary muscle rupture (i.e. post myocardial infarction)
- Spontaneous chordal rupture (in myxomatous mitral valve disease)
- Clinical Picture:
- The classic presentation is a patient who presents with acute pulmonary edema and cardiogenic shock.
- If POCUS is available, MR is usually not seen due to wide-open flow (no “jet”)
- However, the LV will be hyperdynamic
- Patient often has a faint decrescendo early systolic murmur due to rapid equalization of LV-LA pressures (wide open laminar flow, no turbulence to produce murmur)
- If POCUS is available, MR is usually not seen due to wide-open flow (no “jet”)
- The classic presentation is a patient who presents with acute pulmonary edema and cardiogenic shock.
- Diagnosis:
- Urgent echocardiography must be performed to confirm the diagnosis.
- Management:
- Urgent surgical consultation for primary repair of the mitral valve
- Medical therapy can be used to stabilize patients until surgery is arranged
- Afterload reduction to reduce regurgitant fraction
- If the patient is not hypotensive, afterload reduction with short-acting agents can be attempted, which include IV nitroprusside, IV nitroglycerin, and IV milrinone
- However, many patients are extremely hypotensive (MAP < 60mmHg), in which case vasopressors may need to be started for support
- Increase inotropy
- Milrinone or dobutamine can be used to increase cardiac output. These agents can cause hypotension, which can be counteracted with an alpha-agonist (such as norepinephrine).
- Mechanical support
- Intra-aortic balloon pump is a highly preferred temporizing measure
- Promotes forward flow by reducing afterload, reduces MR, and increases diastolic perfusion.
- Intra-aortic balloon pump is a highly preferred temporizing measure
- Afterload reduction to reduce regurgitant fraction
Chronic Mitral Regurgitation
Types of Mitral Regurgitation:
- Primary: mitral regurgitation due to an pathologic problem with the mitral valve apparatus (leaflets, papillary muscle, chordae tendonae, and annulus)
- Secondary: functional mitral regurgitation due to diseases of the ventricle and/or atria, which cause dilation of the valve annulus, and malcoaptation of the leaflets. NOTE: the leaflets themselves are structurally normal.
Causes
- Most common cause of primary MR is degenerative (myxomatous) mitral valve leading to mitral valve prolapse (MVP) and/or flail leaflets.
- Other causes include mitral annular calcification, rheumatic heart disease, coronary artery disease (papillary muscle rupture/dysfunction), endocarditis and collagen vascular diseases.
Hemodynamic Effect
- Chronic mitral regurgitation has a “low afterload, high volume” effect on the LV. A large fraction of blood exits the LV to the low-pressure LA.
- Early stages:
- Rise in LVEF because the ventricle is offloaded in systole into the low-pressure LA. The LV is described as “hyperdynamic”, with EF > 70%.
- LA pressure rises, which can cause dyspnea
- Late stages:
- Volume overload due to reduced cardiac output, and renin-angiotensin activation causing water/salt retention.
- Pulmonary hypertension develops as pulmonary capillaries constrict and remodel in response to high hydrostatic pressures.
- LV dilates due to volume overload
- End stage:
- EF will start to normalize back to 55-60%, and then reduce further.
- Pulmonary congestion/edema, heart failure exacerbations
- Severe MR with low EF is generally an end-stage high-risk problem because repairing the MR will remove the low-pressure exit from the LV, which will worsen the post-operative EF further and can result in cardiogenic shock.
- Surgery should ideally be performed before LVEF falls.
History & Physical
History
- Most patients are asymptomatic in the mild-moderate stages
- Exertional dyspnea, fatigue and weakness are the most common symptoms (due to poor cardiac output and pulmonary hypertension)
- At late stages patients will develop symptoms of pulmonary congestion and edema
Physical exam
- Vital signs: Normo/hypotension, tachycardia, hypoxemia.
- Palpation: displaced apical impulse (dilation of the left ventricle)
- Auscultation: holosystolic murmur heard best over the apex and radiates to the axilla (posterolateral directed MR) or LV base (anteromedial directed MR); if MVP, may hear a midsystolic click
- Minimal respiratory variation (as compared to right sided lesions)
- Louder with increased venous return (passive leg raise) or increased arterial pressure (squat or isometric hand grip)
- Quieter with decreased venous return (Valsalva)
- MVP is a special case, just like with HOCM, where increased venous return will reduce the murmur and delay the click, whereas reduced venous return will increase the murmur and make the click earlier
- Due to redundancy in mitral valve leaflets, which is reduced with larger volume
- Associated findings:
- Pulmonary edema
- R-sided HF (peripheral edema)
- Pulmonary Hypertension
- Note: acute MR may not generator a murmur due to laminar flow between the LV and LA.
Investigations
ECG: left atrial enlargement (p-mitrale), atrial fibrillation
Chest Xray: cardiomegaly, left atrial enlargement
Echocardiography: TTE is the first line test to confirm diagnosis and severity of MR
- Left ventricle is hyperdynamic early in disease, but later dilates and reduces in function later in disease.
- NOTE: Due to the laminar flow, acute MR is difficult to see on color doppler. A hyperdynamic LV in the presence of cardiogenic shock and pulmonary edema suggests acute severe MR.
Important to pay attention to the cause of MR as the management will be different
TEE may be needed to confirm cause
- Other parameters include LV size and function (indications for intervention), left atrial size, and pulmonary hypertension
- Left ventricle is hyperdynamic early in disease, but later dilates and reduces in function later in disease.
Mangement
Asymptomatic MR
- In asymptomatic MR, serial monitoring with echo is indicated, with length of follow-up based on severity of MR
- Asymptomatic severe MR (stage C) should have follow-up echo every 6-12 months to monitor LV function/size and pulmonary pressure
Symptomatic severe MR
Medical Management
- Normal EF:
- Classically afterload reduction has been suggested, which is meant to encourage forward flow and reduce regurgitant fraction
- However, there is little benefit of vasoactive agents in the presence of normal EF
- Reduced EF (< 40%)
- Guideline directed medical therapy indicated for ejection fraction <40% as per CCS
- CRT if the patient has LV dyssynchrony (LBBB with QRS > 130ms)
- CRT re-synchronizes activation of papillary muscles, which can reduce MR
Valve Intervention
- Primary Mitral Regurgitation indications for intervention:
- Severe MR + symptoms (Class 1)
- Severe MR + systolic dysfunction (EF≤60% or End Systolic Diameter ≥40mm) (Class 1)
- Severe MR (No symptoms) Class IIA
- New indication based on the AHA 2020 guidelines
- Many patients with severe MR eventually will have secondary LV dilation and dysfunction
- Studies suggest earlier intervention, provided it is done safely by an experienced operator at a high volume centre (mortality < 1%)
- MV surgical repair preferred over replacement when possible
- Previous guidelines discouraged mitral valve surgery if EF ≤ 30%, citing high risk. However, AHA 2020 guidelines recommend mitral valve intervention because outcomes are much poorer in unoperated patients.
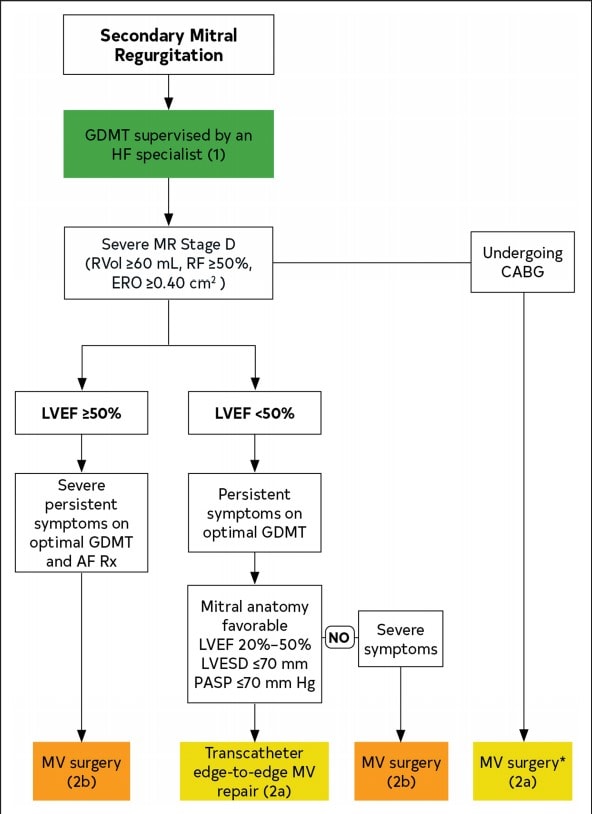
- Secondary Mitral Regurgitation indications for intervention
- First line treatment improves medical management with guideline-directed medical therapy (GDMT) followed by cardiac resynchronization, if eligible
- These therapies can reverse-remodel the LV, reduce mitral annular diameter, and reverse MR by improving coaptation between mitral valve leaflets
- Trans-catheter edge to edge repair strategies (ie. MitraClip) or mitral valve surgery exist, however the benefit is inconsistent across trials (EVEREST, Mitra-FR, COAPT Studies)
- According to the COAPT trial, there may be a benefit in patients with persistent symptomatic secondary MR despite optimal GDMT +/- CRT therapy.
- Patients who have symptoms despite maximally tolerated GDMT should be referred to the heart failure specialist. The “Heart Team” approach includes the primary treating physician, such as an internist, as well as a heart failure specialist.
- First line treatment improves medical management with guideline-directed medical therapy (GDMT) followed by cardiac resynchronization, if eligible
Authors
- Primary Author: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow), Dr. Pavel Antiperovitch (MD, FRCPC, Cardiologist)
- Copy Editor: Megha Shetty, MD Candidate
- Last Updated: Jan. 31, 2022
- For comments or questions, please email feedback@cardioguide.ca