Introduction
- For ECG interpretation and diagnosis of wide complex tachycardia see “Diagnosis of Wide Complex Tachycardia”
- It is important to remember the 5 causes of wide complex tachycardia:
CLASSIC CAUSES OF WIDE COMPLEX TACHYCARDIA - Ventricular Tachycardia
- SVT with aberrancy (usually SVT with RBBB or LBBB)
- Pre-Excitation
- Pacing
- Artifact
(Another commonly cited cause is massive ST elevation)
- When facing a WCT, it is important to remember that VT is the cause in 80% of the cases
- If the patient has ischemic heart disease, then VT is the cause in 90% of the cases.
- General Approach:
- Misdiagnosing SVT as VT would lead to treating with cardioversion and amiodarone. This is aggressive treatment for SVT, but it’s not harmful.
- Misdiagnosing VT as SVT and treating it with IV beta blockers and diltiazem would lead to hemodynamic instability in 100% of the time, thereby producing harm.
- Since a large majority of WCTs are VT (80%), especially in patients with ischemic or structural heart disease, and VT therapies are effective for both VT and SVT, it is more than reasonable to treat all WCT as VT if the diagnosis is uncertain.
Approach
- Assess the hemodynamic stability of the patient
- If unstable, presume VT and treat accordingly
- If stable, monitor continuously, as status can change
- Evaluate ECG features and generate a differential diagnosis
- Narrow the differential using clinical history, physical exam, ECG and diagnostic maneuvers
History / Physical Exam
History:
- Some historical elements can help suggest an etiology of WCT:
- Older patients (>35) are more likely to have VT
- Patients with underlying cardiac disease are more likely to have VT
- Medications:
- Class IA and IC can cause aberration of SVT (by their property of use dependency)
- QTc prolonging agents can predispose to polymorphic VT
- Digoxin most commonly causes VT (monomorphic or bidirectional)
- Symptoms and hemodynamic status are not helpful in establishing the diagnosis in WCT
Physical Exam:
- Look for evidence of heart disease, or manifestation of peripheral vascular disease (e.g., stroke)
- Evidence of AV dissociation on physical exam:
- Variable intensity and appreciation of S1
- Cannon A waves – imply contraction of atrium against a close AV valve (AV dissociation)
- Fluctuation in blood pressure (variation in atrial contribution to end diastolic filling)
Laboratory Investigations:
- Assess for evidence of ischemia (cardiac biomarkers)
- Assess for electrolyte derangement (particularly magnesium and potassium)
- Assess levels of drugs were appropriate (digoxin, antiarrhythmics, etc)
- Toxicology screen
- Some historical elements can help suggest an etiology of WCT:
Diagnostic Maneuvers
Diagnostic Maneuvers
- Only should be done for hemodynamically unstable patients with crash cart ready to deliver cardioversion if necessary.
- Vagal maneuvers – can produce transient AV block, which can terminate some re-entrant SVTs.
- Adenosine
- Very helpful diagnostically to distinguish VT from SVT.
- Adenosine will result in a transient AV block, which may terminate some re-entrant SVTs, or block conduction to the ventricles to reveal atrial activity (such as atrial tachycardia).
- Adenosine generally has no effect on VT.
- Start with 6mg adenosine IV followed by rapid IV saline flush. If no effect, dose is doubled to 12mg IV. If no effect, then can be doubled to 24mg IV.
- With each injection warn the patient about the sensation of adenosine, and check to ensure the IV line is functional.
- No response to 24mg of adenosine generally means the tachycardia is insensitive to adenosine, and does not require the AV node in its mechanism (VT).
- NOTE: Some VT rhythms are adenosine sensitive, particularly outflow tract idiopathic VT.
Acute Management
General Approach
- Determine if patient is stable or unstable
- Unstable patient:
- If patient is unstable but pulse present – Start with synchronized cardioversion when possible, otherwise deliver unsynchronized shock
- If pulseless – begin CPR and deliver high-energy countershock, follow ACLS algorithm
- Stable patient:
- Attempt diagnostic maneuvers as above
- Establish etiology and treat accordingly (below)
- Avoid using IV beta-blockers, CCB or digoxin if etiology of WCT unestablished as it may precipitate hemodynamic collapse
| AHA ALCS Guidelines 2018 |
| AHA Guidelines: Stable Vs. Unstable |
|---|
|
| AHA Definition of “Sustained” VT |
|---|
| AHA 2017 Guideline |
|
Acute Termination of VT:
NOTE: If the patient has stable wide QRS tachycardia, consideration should be given to confirming the diagnosis of VT with adenosine. Otherwise, acute termination options include:
- Electrical cardioversion
- Preferred for hemodynamically unstable or unconscious patients
- Synchronized cardioversion if QRS and T-wave readily discernible; otherwise, unsynchronized cardioversion (according to ACLS)
- If the patient is awake sedation MUST be administered. Generally midazolam (+/- fentanyl) is preferred in this case due to minimal effects on blood pressure. Ketamine is also an option, but is less frequently used due to emergence reactions.
- ***IMPORTANT NOTE: Electrical cardioversion should never be performed on a conscious patient. A conscious patient has enough cardiac output to perfuse the brain, and can tolerate sedation. If they do not tolerate sedation and become unstable/unconscious, then an urgent cardioversion is indicated. Cautious use of phenylephrine can help offset the vasodilating effect of sedatives and should be ready to be given as boluses during sedation of hypotensive patients.
- Pharmacological cardioversion
- Preferred in patients with stable sustained VT
- Procainamide
- Loading dose: 20-50mg/minutes until arrhythmia stops or a maximum dose of 17mg/kg is delivered. Maintenance dose at 1-4mg/minute
- More effective than Amiodarone (PROCAMIO trial)
- Can be used for ischemic and non-ischemic cardiomyopathy
- Amiodarone
- Dose: 150mg IV over 10 minutes, followed by 1mg/minute for 6 hours, then 0.5mg/minute for 18 hours (or can switch to oral). Total: 900mg (1 bag)
- Most commonly used, as clinicians are most familiar with it
- Lidocaine:
- Dose: 1-1.5 mg/kg bolus, can repeat a 0.5-0.75mg/kg bolus q5-10 minutes (for a maximum dose of 3mg/kg), then follow by a continuous infusion at 1-4mg/minute
- Less effective of the 3 options, and often added as an adjunct to Procainamide or Amiodarone.
- Theoretically more effective in ischemic VT (in cells with metabolic acidosis).
- NOTE: Oral version of IV lidocaine is mexiletine.
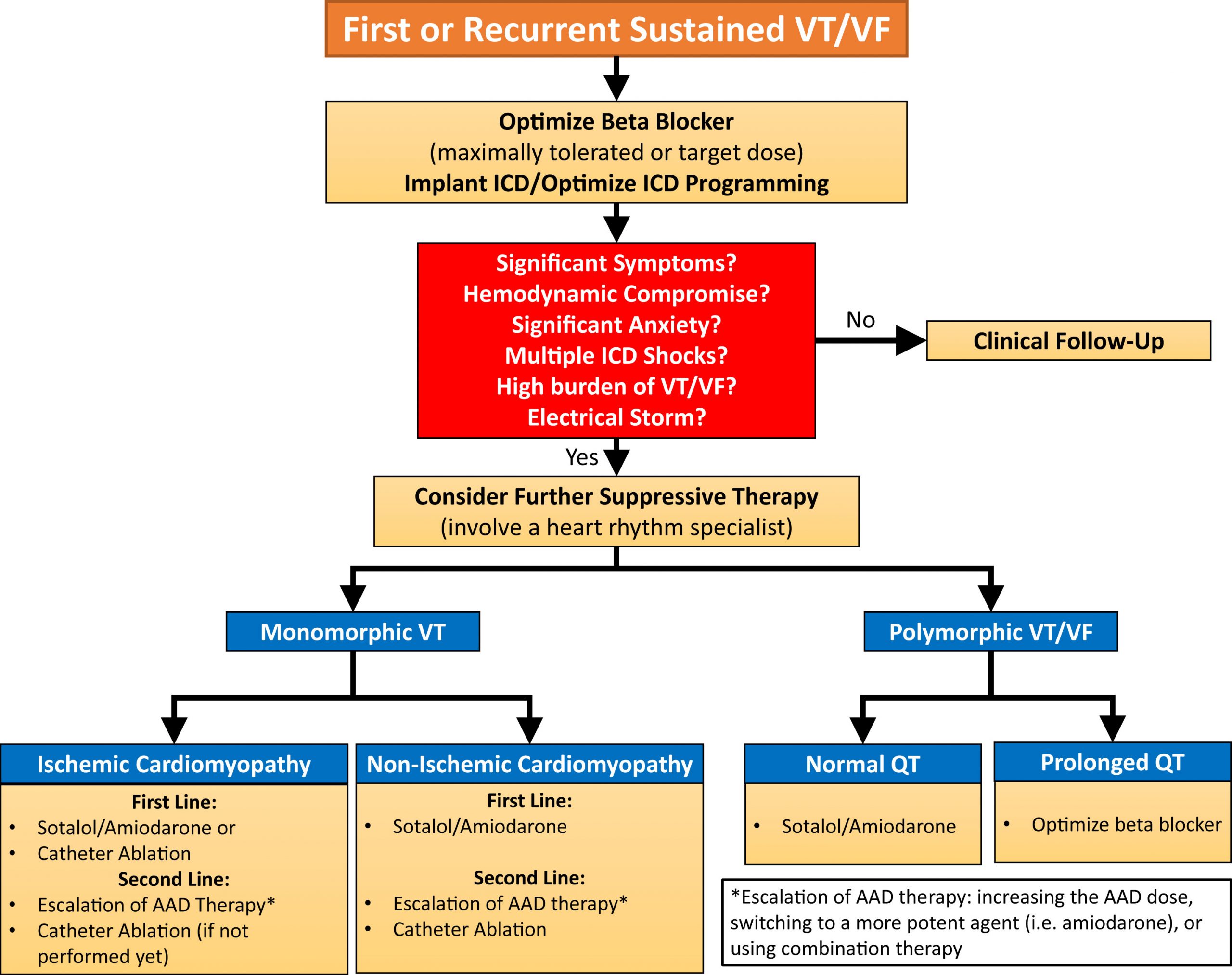
Treatment of VT Storm:
| VT Storm Definition (AHA 2017) |
|---|
| VT/VF storm (electrical storm or arrhythmic storm) refers to a state of cardiac electrical instability that is defined by ≥3 episodes of sustained VT, VF, or appropriate shocks from an ICD within 24 h |
- Once patient is out of VT, there are THREE pillars of VT storm management to prevent further VT:
- Anti-Arrhythmic Medications:
- Amiodarone (most common)
- Procainamide (most effective)
- Lidocaine (least effective, fewest side effects)
- Beta-blockade
- Propranolol PO 40mg q6hours for first 48 hours)
- Best evidence from RCT
- More effective than metoprolol (Chatzidou et al 2018 JACC)
- Metoprolol PO up to 100mg BID or 60mg TID PO
- Esmolol IV: 0.5 mg/kg bolus, 0.05 mg/kg/min
- Easily titratable (halflife is 9 min)
- Best choice if patient is hemodynamically unstable.
- Propranolol PO 40mg q6hours for first 48 hours)
- Sedation
- NOTE: this is an extremely important, and most often forgotten step
- The patient must be RAAS -1 or -2 (Wakes to speak with you, but falls asleep when you leave the room)
- Benzodiazepines (common choices are lorazepam 1-3mg q8h or midazolam IV 1-2mg/hr)
- Propofol (most effective anti-arrhythmic), but requires intubation if patient is too sedated
- Other: Treat underlying substrate
- Remove offending agents (QTc prolonging drugs)
- Correct electrolyte derangements
- Revascularization in acute ischemia
- NOTE: Revascularization for patients with VT storm
- Monomorphic VT is usually caused by a macro-reentry circuit involving areas of scar in patients with poor LV function (< 30-35%). In rare cases, VT can be triggered by ischemia.
- In the absence of objective evidence of ongoing ischemia, urgent angiography is of limited value in the acute treatment of VT storm.
- However polymorphic VT and VF are frequently caused by ischemia, and urgent revascularization may be of benefit.
- Anti-Arrhythmic Medications:
Refractory VT Storm
- Options for VT storm refractory to medical therapy:
- Sedation with propofol and intubation
- Sedation with propofol is highly effective in settling electrical storm. Intubation may be indicated for airway protection if higher doses of propofol are needed.
- Ensure all discussions of goals of care, cardiac transplantation, and potential ablation procedures are completed prior to sedation.
- Cardiac Transplantation
- This is definitive management for a patient in VT storm. A discussion about cardiac transplantation MUST be initiated as early as possible because a transplant assessment and workup must be completed.
- Goals of care discussion
- Especially important if the patient is > 70yo and unlikely to be eligible for cardiac transplantation.
- Catheter ablation
- Overall ablation can be attempted as a bailout procedure. It may have limited efficacy, especially in patients with large amount of scar burden or non-ischemic cardiomyopathy, which have patchy scar with numerous foci of VT substrate.
- Ablation may not be possible if the patient is too unstable to tolerate catheter access of the left ventricle.
- Stellate Ganglion block and Sympathetic Denervation (option in centres experienced in stellate ganglion blockade and
- Sedation with propofol and intubation
Patients with pacemakers/ICD:
- Pacemaker mediated tachycardia (PMT) is a rare form of WCT in patients with a dual chamber pacemaker. The pacemaker tracks a retrograde A from the prior V-pace to create a re-entry loop, or a pacemaker is rapidly pacing the V in an attempt to track an intrinsic atrial arrhythmia.
- Patients with suspected pacemaker mediated tachycardia (PMT) can be easily treated by temporarily applying a magnet to the device. The magnet will activate “magnet mode”, which will disable sensing and revert pacemaker function to asynchronous fixed-rate mode (usually 80 bpm). This will terminate any PMT rhythms, and the patient should revert to normal rhythm once magnet is removed.
- NOTE: PMT is uncommon in modern medicine due to various anti-PMT device algorithms.
- When a patient has a pacemaker, and presents with WCT you can easily rule out PMT by applying a magnet to the device.
Further Reading
- 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death
- 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society Position Statement on the Management of Ventricular Tachycardia and Fibrillation in Patients With Structural Heart Disease
- Issa, Z. F., Miller, J. M., & Zipes, D. P. (2019). Clinical Arrhythmology and Electrophysiology. Philadelphia, PA: Elsevier.
Authors
- Primary Authors: Dr. Yehia Fanous (MD, Internal Medicine Resident), Dr. Pavel Antiperovitch (MD, FRCPC, EP Fellow)
- Author/Reviewer: pending
- Staff Reviewer: pending
- Copy Editor: pending
- Last Updated: Dec 14, 2020
- Comments or questions please email feedback@cardioguide.ca