Abbreviations
- TTE: trans-thoracic echocardiography
- TEE: trans-esophageal echocardiography
- PMBC: percutaneous mitral balloon commissurotomy
- PASP: pulmonary artery systolic pressure
- TAVI: transcatheter aortic valve implantation
Introduction
- Options of fixing stenotic valves include percutaneous vs. open and valvuloplasty vs. replacement
- Decision should involve a Valve Team and is individualized to every patient
- Patient profile and technical factors influence decision
- Choosing what type of intervention will be the focus of this article. Diagnosing stenotic lesions and medical therapy are discussed here.
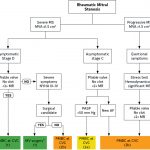
Rheumatic Mitral Stenosis
Diagnosis
- TTE is indicated to establish diagnosis and TEE if percutaneous mitral balloon commissurotomy (PMBC) is being considered
- If discrepancy between clinical and echocardiographic parameters, exercise testing or cardiac catheterization can be done
Criteria
- Severe mitral stenosis is diagnosed by:
- Mitral valve area <1.5 cm2
- Calculated by planimetry or diastolic pressure half time (>150 ms)
- Mean gradient usually above 5-10 mmHg (at normal heart rate)
- Varies by heart rate thus not included in definition
- Ancillary findings:
- Severe LA enlargement
- Elevated pulmonary artery systolic pressure (>50 mmHg)
- Mitral valve area <1.5 cm2
Interventions
- Percutaneous mitral balloon commissurotomy (PMBC)
- Indicated in patients with:
- Pliable valve, no clot, <2+ MR with symptoms OR
- No symptoms and high PASP (>50 mmHg) OR
- New AF
- Indicated in patients with:
- Mitral Valve Surgery
- Surgical commissurotomy preferred vs mitral valve replacement
- Indicated in patients with severe symptoms (NYHA III or IV) who are surgical candidates
- Trans-catheter valve implantation of TAVI bioprosthesis
- If not a PMBC or surgical candidate
PMBC
- TTE for diagnosis of severe MS and TEE to look for thrombus and severity of MR
- Goal is to use a balloon to split the commissures (instead of splitting the valve)
- Good candidates have pliable valves:
- Crisp opening snap and loud S1
- Wilkins Score <8
- No calcium in commissures
- Contraindications
- Moderate or greater MR
- LA thrombus
Mitral Valvuloplasty (Wilkins/MGH) Score
- Wilkins score 8 or less predicts a favorable result but a score greater than 8 does not preclude PMBC
- Calculator
Non-Rheumatic Calcific Mitral Stenosis
- Though rheumatic mitral stenosis is the most common cause of mitral stenosis, calcific mitral stenosis is becoming more common in elderly populations
- In contrast to rheumatic, calcification starts at the base and usually spares the leaflet tips
- No commissural fusion
- Determination of severity is difficult as planimetry is challenging
Interventions
- No role for PMBC or surgical commissurotomy
- Surgery is technically challenging as mitral annular calcification causes difficulty in securing a prosthesis
- Guidelines recommend valve intervention in patients with severe symptoms (NYHA III or IV), severe mitral stenosis (mitral valve area < 1.5 cm2) and after discussion of the high operative risk with the patient
Further Reading
Authors
- Author: Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Copy Editor: Megha Shetty (MD Candidate)
- Last Updated: April 5, 2021
- Comments or questions please email feedback@cardioguide.ca