Abbreviations
- OAC – Oral anticoagulant (includes warfarin, NOACs, etc.)
- DAPT – Dual anti-platelet therapy
- PPI – Proton pump inhibitor
- CCS – Canadian Cardiovascular Society
- AHA – American Heart Association
- CCS – Canadian Cardiovascular Society
- ARB – Angiotensin receptor blocker
- ACEi – ACE inhibitor
- BB – Beta blocker
- FFR – Fractional flow reserve
Pillars of post-MI care
- Determine need for further revascularization
- Optimize medical therapy
- Risk factor modification
- Cardiac rehab
- Arrange appropriate follow-up
Determine a need for further revascuarlization
- If there are ongoing signs/symptoms of ischemia, further revascularization of potential flow-limiting non-culprit lesions can be considered.
- Controversy has existed about “bystander” lesions found during a STEMI that are significant (either visually > 70% stenosis or by FFR). Latest trials recommend complete revascularization either during index PCI procedure or as a staged procedure. Decision is made with the interventional cardiologist.
- Post-STEMI – Culprit-only PCI at time of STEMI and consider complete revascularization in 2-30 days based on visual assessment of stenosis and FFR (COMPLETE, PRAMI, CULPRIT favour complete revasc)
- Patients in shock – Culprit-only PCI at time of STEMI (CULPRIT-SHOCK Trial)
CULPRIT-SHOCK Trial
In patients with acute MI with multi-vessel CAD and cardiogenic shock culprit-only PCI is associated with 9.5% absolute reduction in the rate of death or renal replacement therapy at 30 days. This was driven primarily by a 7.3% absolute reduction in all-cause mortality with culprit-lesion only PCI.
Anti-Thrombotic Therapy
- Patients should remain on dual antiplatelet therapy post-MI
- ASA, ticagrelor, clopidogrel, and prasugrel all have mortality benefit post-MI
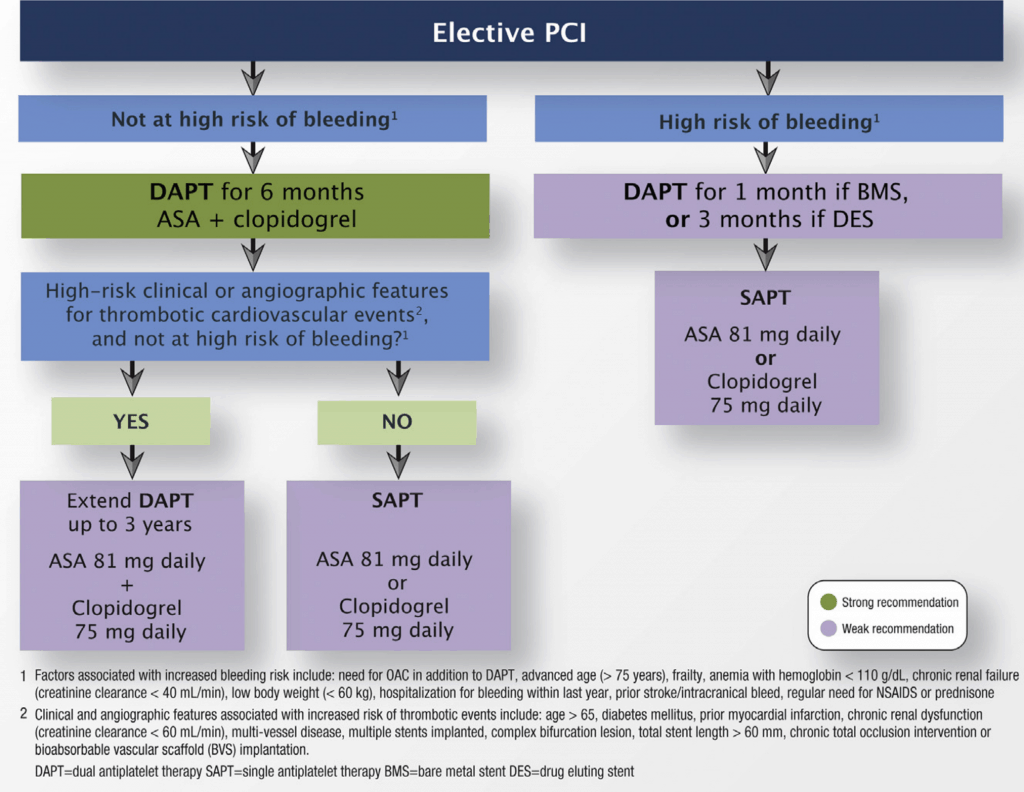
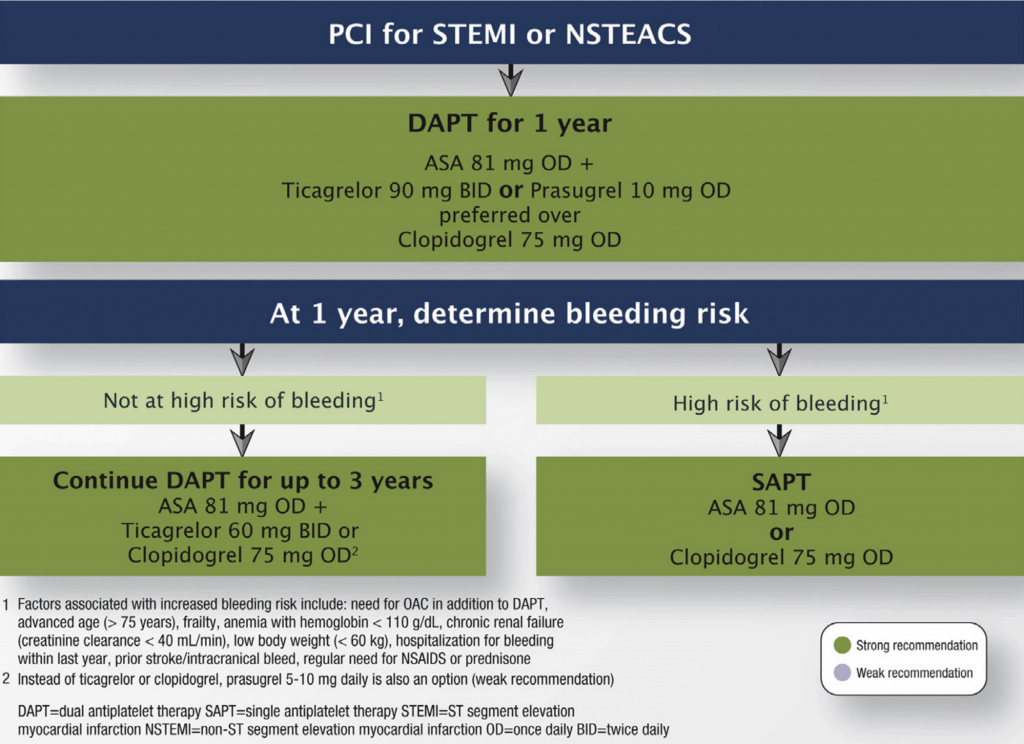
- Optimal duration:
- STEMI or NSTEMI: At least 1 year (CCS)
- Elective PCI (Outpatient): At least 6mo (CCS)
- There is evidence to continue >1 year
- At 1 year, weigh risks of bleeding vs. risk of ischemic events (See Table to the right)
- Generally, if tolerating DAPT at 1 year post-MI, continue for up to 3 years with one of the following proven regimens:
- ASA 81 mg daily + ticagrelor 60 mg BID (REDUCED DOSE) (PEGASUS-TIMI-54 Trial)
- ASA 81 mg daily + clopidogrel 75 mg daily (DAPT Trial)
- ASA 81 mg daily + prasugrel 10 mg daily (DAPT Trial) – not available in Canada
Interruption of antiplatelet therapy
- Reasons to consider early interruption (<1 year) of therapy in patients with a stent:
- High-risk of bleeding
- Elective non-cardiac surgery
- Semi-urgent non-cardiac surgery
- CABG (urgent or elective)
- Continue ASA monotherapy through surgery if possible
- Early interruption increases risk of stent thrombosis
- Resume DAPT post-op once “deemed safe by the surgeon” (CCS 2018)
| CCS 2018 Antiplatelet Guidelines |
| Interruption of antiplatelet therapy |
|---|
|
- CABG (special case):
- Continue ASA peri-operatively (operate on ASA)
- Ticagrelor and clopidogrel: interrupt at least 48-72hrs pre-CABG (ideally 5 days)
- Prasugrel: interrupt at least 5 days pre-CABG (ideally 7 days)
- Urgent cases: try to wait at least 24hrs (sometimes wait not possible)
- Overall, weigh risks of bleeding and thrombosis. Include others in the decision (surgeon, cardiologist, attending physician)
Switching antiplatelet therapy (CCS 2018)
- Do not switch unless compelling reason to do so (stent thrombosis, bleeding, side effects, etc.)
- Clopidogrel → Ticagrelor (load 180 mg + 90 mg BID regardless of last dose)
- Ticagrelor → Clopidogrel (load 600 mg at time of next ticag dose) (OPTI-CROSS Trial)
- Do not load when switching from prasugrel (see CCS 2018 guideline)
- Clopidogrel → Prasugrel (load 60 mg + 10 mg daily regardless of last dose)
- Prasugrel → Ticagrelor (do not load, give 90 mg BID at time of next dose)
- Ticagrelor → Prasugrel (load 60 mg + 10 mg daily at time of next dose)
- Prasugrel → Clopidogrel (do not load, give 75 mg at time of next dose)
ACS in patient with atrial fibrillation
Atrial fibrillation ACS or high-risk PCI:
- ASA + clopidogrel + reduced-dose OAC (aka “triple therapy”)
- ASA can be discontinued from 1 day after PCI to 6 months. (In clinical trials, clinicians converted triple therapy to dual therapy after 1-3 weeks. Interventionalist will generally dictate duration.)
- Once ASA discontinued, patient continues on clopidogrel + OAC (aka “dual therapy”)
- NOTE: The dose of OAC depends on whether it is used for triple or dual therapy (see below).
- OACs regimens tested in triple therapy:
- Rivaroxaban 2.5 mg BID + ASA + clopidogrel
- Warfarin (target INR 2.0-2.5) + ASA + clopidogrel
- Apixaban 5 mg BID + ASA + clopidogrel
- OACs tested in dual therapy:
- Rivaroxaban 15 mg daily + clopidogrel (PIONEER)
(Rivaroxaban 10 mg in renal dysfunction) - Dabigatran 150 mg BID + clopidogrel (RE-DUAL trial)
(Dabigatran 110 mg BID = lower bleeding, trend towards ischemic events) - Apixaban 5 mg BID + clopidogrel (AUGUSTUS Trial)
*use low-dose apixaban 2.5 mg BID if 2 of: age < 80, weight < 60 kg, creatinine > 133 umol/L
- Rivaroxaban 15 mg daily + clopidogrel (PIONEER)
- Notes:
- Use PPI with triple therapy.
- Clopidogrel is safest in combination with OAC (dual or triple therapy). Less data with ticagrelor.
- Routine triple therapy is not recommended for prevention of LV thrombus in anterior MI (CCS 2018 guideline).
- All above reflects chronic management post-ACS/stenting. However, patients actively treated for acute coronary syndromes should still be treated with DAPT and IV/SC anticoagulation, which has proven benefit in acute coronary syndromes. OAC is often held in these situations, and restarted once need for IV/SC anticoagulation resolves.
Adjunctive Therapy
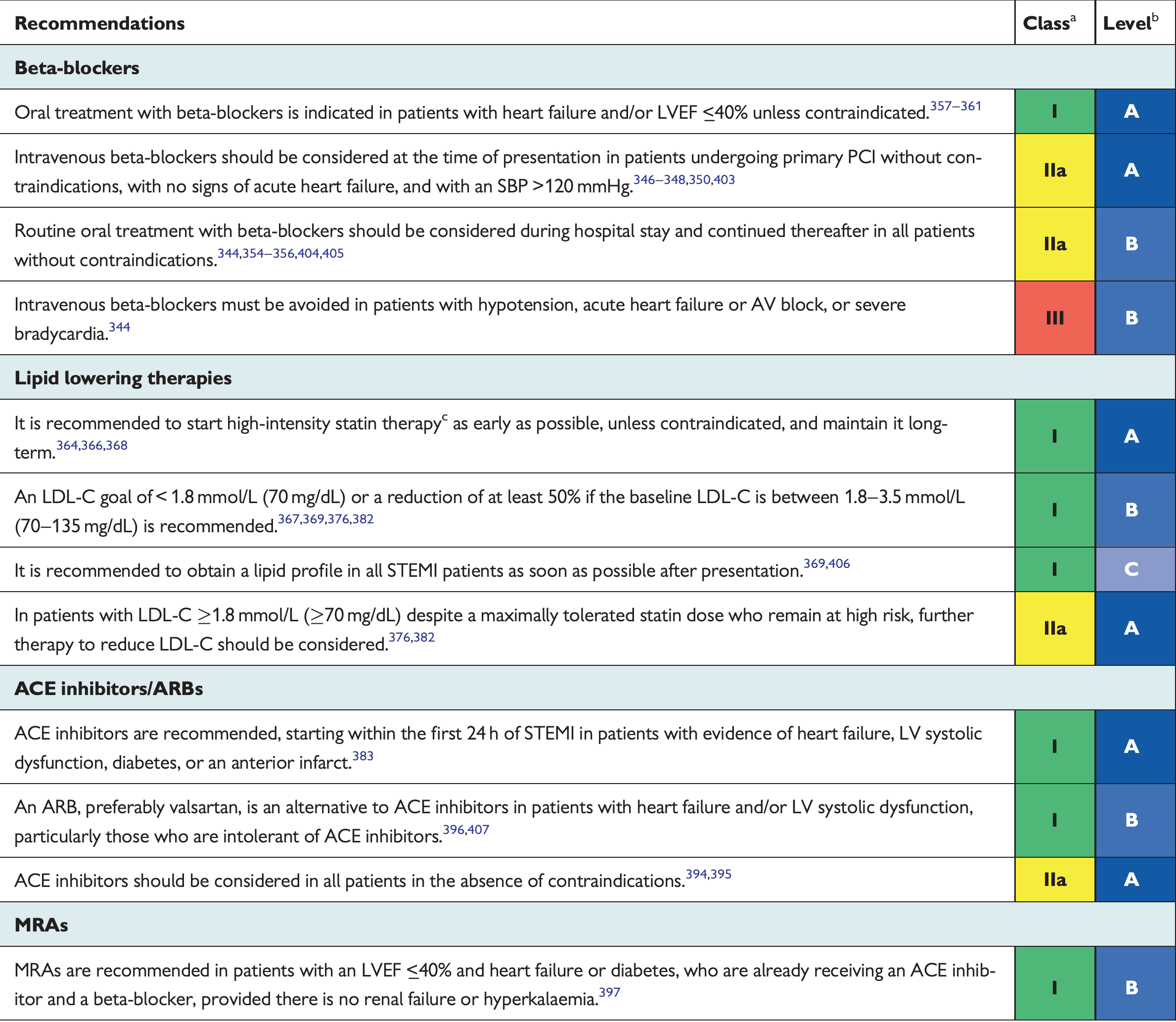
Beta Blockers
- Indications: Start within 24 hours of ACS diagnosis (unless contraindication), continue for at least 3 years [Class I]
- Benefits: Reduce ischemia, re-infarction, arrhythmias, mortality.
- Acutely in MI: Benefits controversial, more benefit in chronic post-MI care
- Trials: TIMI-2B Study, BHAT (mortality benefit), COMMIT (no benefit), (N Engl J Med. 1983; 308:614–8)
- Options/Doses:
- If no LV dysfunction (post-MI prevention): Metoprolol 12.5 mg BID, atenolol 12.5-25 mg OD, benefit extrapolated to bisoprolol 2.5 mg OD
- If LV dysfunction: Bisoprolol 2.5 mg daily, carvedilol 3.125 mg BID, metoprolol 12.5 mg BID
- If contraindicated: Re-evaluate in 24 hours
- Contraindications: (if contraindicated, re-evaluate in 24hrs)
- Acute heart failure (risk of precipitating cardiogenic shock)
- Evidence of low-output state / cardiogenic shock
- AV block: 3rd/2nd degree, PR interval > 240ms
- Severe asthma/COPD
ACE Inhibitors
(use ARB if ACEi-intolerant)
- Indications: Proven benefit in post-ACS patients with ANY of: EF < 40%, HTN, DMII, or CKD [Class I], but benefit extrapolated to all ACS within 24hrs [Class IIB]
- Trials: SAVE, AIRE, HOPE
- Options/Doses:
- Ramipril 2.5-5 mg OD (titrate to 10 daily – AIRE study)
- Perindopril 2 mg OD (titrate to 8 mg – PREAMI study)
- Enalapril (CONSENSUS II – no benefit)
- Indications: Proven benefit in post-ACS patients with ANY of: EF < 40%, HTN, DMII, or CKD [Class I], but benefit extrapolated to all ACS within 24hrs [Class IIB]
Mineralocorticoid Receptor Antagonists (MRA)
- Indications:
- Need all of: On max dose ACEi, BB, and post-MI + EF ≤ 40% + (HF symptoms or DMII) [Class I]
- CCS 2017 HF Guideline: “MRA for patients with acute MI with EF < 40% and HF or with acute MI and an EF < 30% alone in the presence of diabetes”
- Trial: EPHESUS
- Need all of: On max dose ACEi, BB, and post-MI + EF ≤ 40% + (HF symptoms or DMII) [Class I]
- Options/Doses:
- Eplerenone 25 mg daily (titrate up to 50 mg daily)
- Contraindications (for post-MI indication):
- Creatinine > 221 (men), > 176 (women)
- K+ > 5.0
- Indications:
- Calcium channel blockers (diltiazem/verapamil)
- 2nd line to beta blockers (if ongoing ischemia), reduce re-infarction
- Negative inotropes → contraindicated in LV dysfunction
- Indicated for coronary artery spasm
High-Intensity Statins
- Indications: All ACS patients [Class I]
- Benefits: Reduces recurrent MI, CV mortality, need for revascularization, and stroke
- Trials: PROVE IT-TIMI 22, MIRACL, TNT (high dose)
- Options/Doses:
- Atorvastatin 40-80 mg
- Rosuvastatin 20-40 mg
- Pravastatin and simvastatin are not high-intensity statins.
- ESC 2017 STEMI recommendations for post-MI care
- NOTES:
- NSAIDs contraindicated post-MI (increases risk of MACE)
- All admitted NSTEMI patients need 24 hours of rhythm monitoring (or until revascularization), and only select UA patients
- STATIN-indicated conditions: (conditions that require statin use as per CCS 2021 Lipid Guidelines)
- LDL ≥ 5.0 mmol/L
- Most patients with diabetes (Age ≥ 40 or ≥ 30 and ≥ 15y of DM duration)
- ASCVD (MI/ACS, Stable Angina, coronary artery disease, Stroke, TIA, PAD, AAA)
Cardiac Rehab
- Cardiac rehab for all ACS patients
- Benefits:
- Risk factor modification:
- Lipid profile improves
- More effective smoking cessation
- Improves glycemic control in diabetes
- Improves symptoms
- Improves functional capacity (improves O2 delivery and reduces utilization)
- Improves mortality by 20% post-MI (especially after PCI and CABG)
- Psychological
- Improves self-confidence and anxiety/depression (patients feel healthy after coronary events, more likely to return to work/exercise)
- Risk factor modification:
- Complications:
- Ventricular fibrillation, myocardial infarction, sudden death (but risk is low, attributed to poor surveillance
- Benefits:
Counselling
- Medication adherence
- Follow-up plan
- Smoking cessation (counselling should be initiated in hospital and followed up at 3 months as outpatient)
- Dietary advice
- Physical activity
- Primary Author: Dr. Pavel Antiperovitch (MD, FRCPC, Cardiology Fellow)
- Author/Reviewer: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Staff Reviewer: Pending
- Copy Editor: Perri Deacon (medical student)
- Last Updated: March 22, 2020