Case 1
54M with no medical history presents with 30 minutes of chest pain and brought straight to ED by EMS. Cath lab en route.
VS: HR 105, BP 130/80, RR 20, 98% on RA
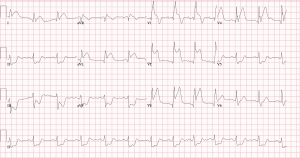
ECG:
Question: Would you give this patient IV beta blocker right now and if so, what dose?
You decided not to use IV Beta blockers because of institutional practises. Successful PCI to prox LAD (TIMI 3 flow). LVgram shows preserved EF. Now
You decided not to use IV Beta blockers. Successful PCI to prox LAD (TIMI 3 flow). LVgram shows preserved EF. Now its 24 hours post cath. VS similar. Is a Beta Blocker indicated in this patient and, if so, are there any contraindications?
No history of reactive airway disease, no heart failure and here is his ECG.
Turns out that was not his ECG and his PR is actually <240 so you start Metoprolol 25mg BID. Echo comes back with EF 50%. Would an ACE Inhibitor be indicated?
What are the indications for a MRA and what are the contraindications (be specific)?
Would you start an MRA in this patient?
He is discharged on Metoprolol 25mg BID and Perindopril 4mg qHS. You see the patient in clinic in 3 years. His Echo shows EF 55-60%. VS HR 63, BP 118/70, RR16, SAT 99% on RA. He denies any side effects from his medications.
He asks if he can come off of any of his medications?