- Atrial fibrillation
- Mitral annular calcification (moderate or greater)
- Mitral stenosis (any) or mitral regurgitation (moderate or greater)
- Mitral valve repair or prosthetic mitral valve
- Left bundle branch block or ventricular paced rhythm
Diastole is made off four phases
- Isovolumetric relaxation time or IVRT (end of AV flow to rapid early filling)
- Passive filling (E-Wave)
- Diastasis (end of passive filling, equalization of pressure in LV and LA)
- Atrial Contraction (A-wave)
- We can visualize this with echo using a PW doppler just above the MV leaflets in the Apical 4 Chamber

Diastolic dysfunction: generally caused by impaired LV relaxation, reduced restoring forces, and increased LV thickness

Elevated LV Filling Pressures (pressures in the left ventricle during diastole) without increased volumes is suggestive of diastolic dysfunction.
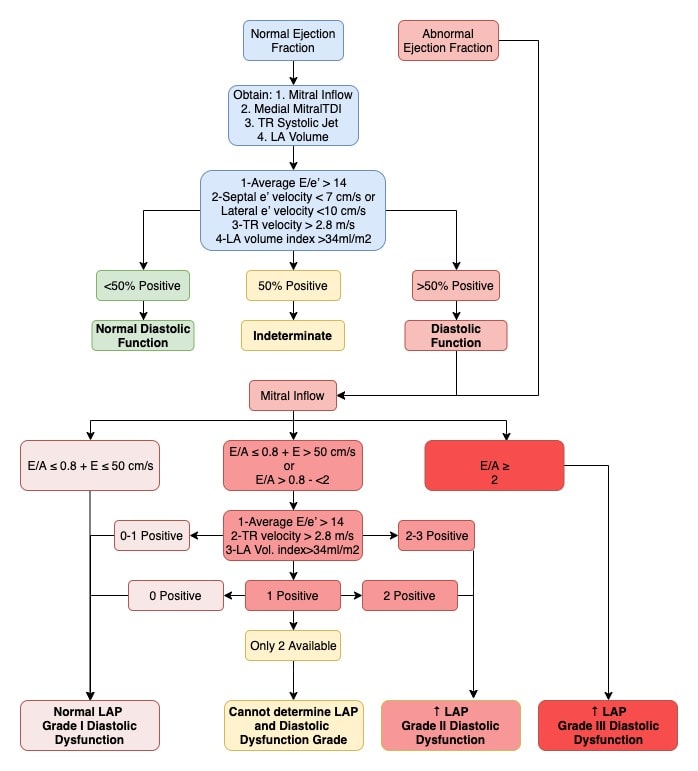
- Mitral Inflow PW Doppler (Example)
- Measure just above mitral valve leaflets in apical four chamber
- E-wave velocity:
- A-wave velocity:
- E/A ratio:
- Medial Mitral Annulus PW TDI (Example)
- e’ velocity:
- TR Systolic Jet Velocity (Example)
- Parasternal or apical 4 chamber highest velocity CW Doppler of TR jet
- LA Volume Index (Example)
- Calculate biplane volumes by measuring LA in apical 4 chamber and apical 2 chamber then index to BSA
Coming Soon
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European heart journal cardiovascular Imaging. 2016; 17(12):1321-1360.
- https://www.123sonography.com/diastolic-function-and-diastolic-dysfunction
- Aurigemma GP, Gaasch WH. Diastolic Heart Failure N Engl J Med. 2004; 351(11):1097-1105.