Introduction
- Coronary artery disease is the pathologic process of accumulation of atherosclerotic plaque in the epicardial arteries resulting in reduced myocardial blood flow/perfusion and accelerated by certain risk factors.
- Patients with suspected CAD should undergo workup consisting of blood work, echocardiography and risk stratification with non-invasive imaging.
- Treatment goals are to improve symptoms/quality of life, survival, and prevent complications.
- Mainstays of treatment are lifestyle changes and medical management (targeting prognosis and symptoms).
- Revascularization on top of medical management is reserved for a select group of patients with refractory symptoms or anatomy with proven survival benefit.
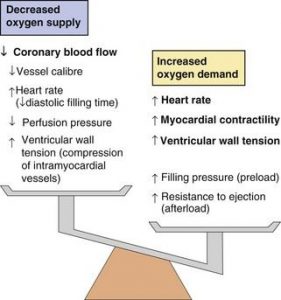
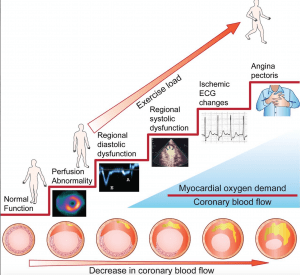
Pathophysiology
- When approaching CAD, its important to keep in mind the ischemic cascade with initial changes being perfusion abnormalities, diastolic and systolic dysfunction, ECG changes and then symptoms as the final step.
Presentation
Risk Factors
Modifiable
- Smoking history
- Dyslipidemia
- Diabetes
- Hypertension
- CKD
- Physical inactivity
- Diet
- Obesity or metabolic syndrome
- Depression
Nonmodifiable
- Age
- Sex (ongoing research on the change in risk for transgender persons)
- Family history of premature CAD
- First degree relative
- Men < 55
- Women < 65
- Ethnic origin
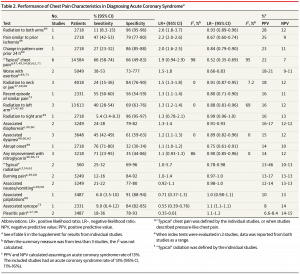
History
- Typical angina is characterized by 3/3 of the following:
- Retrosternal discomfort/ache/heaviness
- Provoked by exertion or emotion/stress
- Relieved within 5 minutes of rest or nitroglycerine use
- Atypical chest pain 2/3 and non-cardiac 1/3 of the above criteria
- Non-classical symptoms are common, especially in diabetics/elderly/transplant patients; more recent studies show most patients present with atypical and non-cardiac chest pain
- Sex differences in presentation are actively being researched, so note that women may present with different symptoms (ie. arm/shoulder/abdo pain)
- Physical exam has a low sensitivity for detection of CAD but important to access for risk factors (such as dyslipidemia or hypertension), complications and other diagnoses
- Rule out unstable angina:
- i. Rest pain
- ii. New onset of CCS3/4 angina
- iii. Crescendo (more frequent, longer or on less exertion
- If unstable, refer to the ACS algorithm (NSTEMI | STEMI)
CCS Class
Class 1: Angina only with strenuous exertion. Presence of angina during strenuous, rapid, or prolonged ordinary activity (walking or climbing the stairs).
Class 2: Angina with moderate exertion. Slight limitation of ordinary activities when they are performed rapidly, after meals, in cold, in wind, under emotional stress, or during the first few hours after waking up, but also walking uphill, climbing more than one flight of ordinary stairs at a normal pace, and in normal conditions.
Class 3: Angina with mild exertion. Having difficulties walking one or two blocks, or climbing one flight of stairs, at normal pace and conditions.
Class 4: Angina at rest. No exertion needed to trigger angina.
Differential Diagnosis (CCS)
Cardiovascular
- Aortic dissection
- CHF
- Pericarditis
Pulmonary
- Pulmonary embolism
- Pneumothorax
- Pleural effusion
GI
- Esophagitis
- Esophageal spasm
- Biliary colic
- PUD
- Pancreatitis
Chest Wall
- Costochondritis
- Fibromyalgia
- Rib fracture
Neuro
- Cervical disease
- Herpes Zoster
Psych
- Anxiety
- Panic disorder
- Hyperventilation
Workup
Basic Investigations (CCS)
- Lab work: Hemoglobin, lipid panel, fasting glucose, hemoglobin A1C, renal function tests, liver function tests, thyroid function tests
- 12-lead ECG
- Transthoracic Echocardiography (ESC Class I)
- Exclusion of alternative causes of angina
- Identification of regional wall motion abnormalities suggestive of CAD
- Measurement of LVEF for risk stratification
- Evaluation of diastolic function
- Chest X-ray if atypical presentation, possible HF or suspicion of pulmonary disease
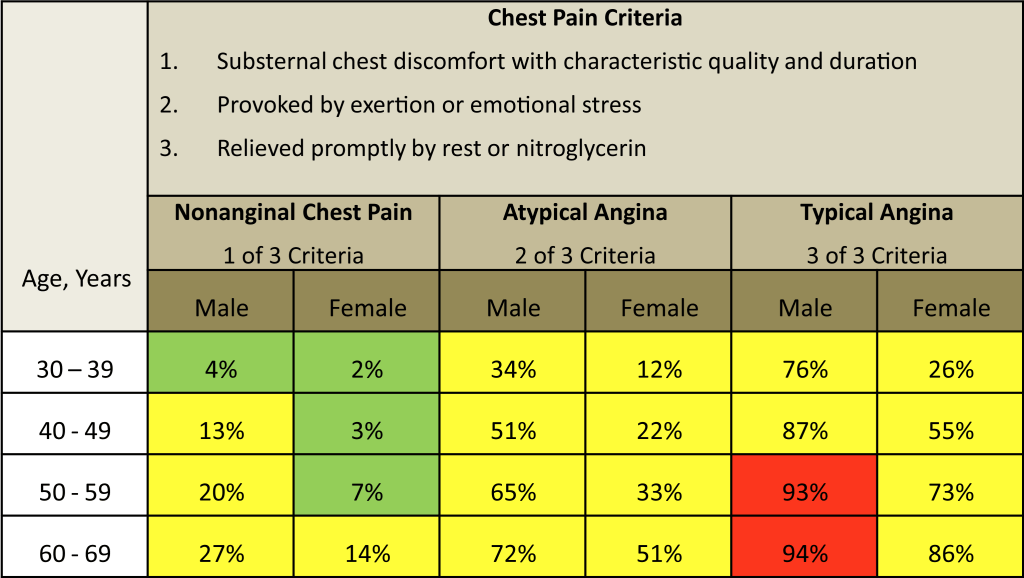
Determine Pre-Test Probability (PTP)
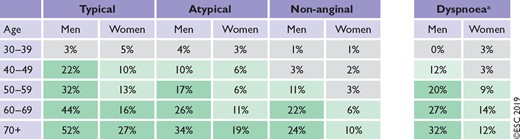
PTP based on chest pain. Other factors that modify risk (ie. q waves on ECG, wall motion abnormalities on echo, and risk factors) should be taken into account as well.
Non-Invasive Diagnostic Testing
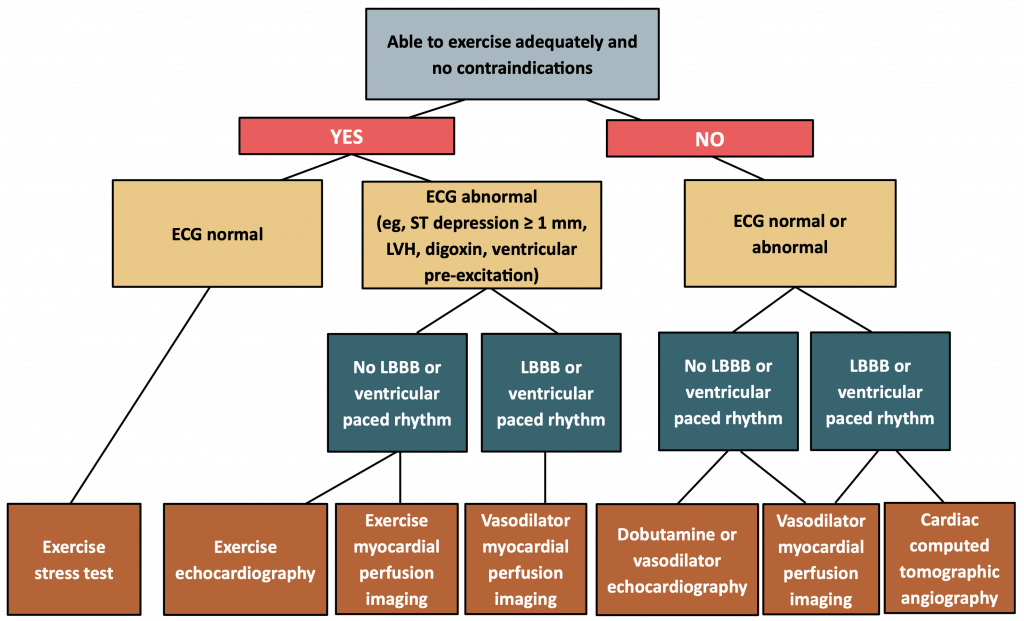
- Exercise, as modality of stress, always preferred given more physiological and added benefit of understanding patient exercise tolerance
- Exercise ECG stress test, though first line for many years, inexpensive, and readily available, is no long considered first line given limited sensitivity and specificity (remember ischemic cascade)
- First line: Echo or Myocardial Perfusion imaging (ideally exercise but if unable, pharmacologic)
- Coronary CT can also be considered in a lower pre-test probability patient given high sensitivity or to assess for left main disease, but should not be used in a high pre-test probability patient given limited specificity.
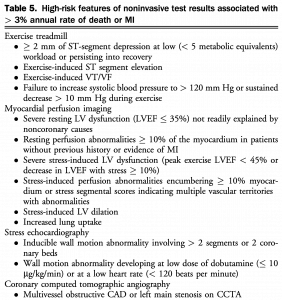
Risk Stratification
|
Management
Goals of Therapy
- Improve symptoms and quality of life
- Improve prognosis, survival
- Prevent non-fatal complications (MI, VT/VF, HF)
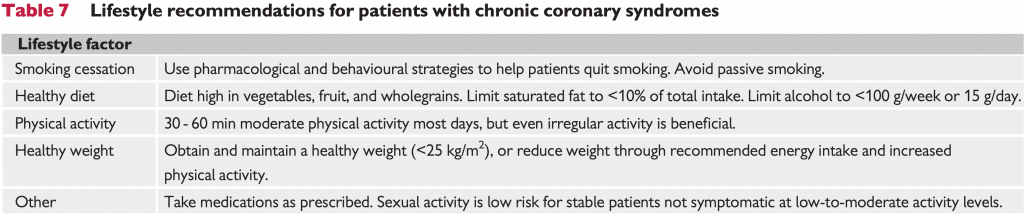
Lifestyle Management
Medical Management
Note: Medical management is the cornerstone of therapy and should be started in all patients with CAD. Invasive coronary angiography is reserved for a select group of patients and will be discussed further below.
Improve Prognosis
- ASA
- Plavix if ASA intolerant (routine DAPT not recommended)
- Statin (other lipid agents if not statin tolerant such as ezetemibe or PCSK9 inhibitors)
- ACE Inhibitor (Consider in all patients with CAD and recommended in those with HTN, diabetes, rEF, and CKD)
- Beta blocker in patients with reduced EF
- Optimize diabetes
- Target A1c <7% (Guideline)
- First line metformin and then choose antihyperglycemics (liraglutide, empagliflozin, and canagliflozin) with proven CV benefit in patients with diabetes (guideline)
- Note: dapagliflozin did not show improved CV mortality (DECLARE TIMI-58) but would be a reasonable choice if HF is predominant issue (DAPA-HF)
- Optimize hypertension
- Quit smoking
- Counselling in combination with pharmacotherapy (ie. varenicline, bupropion, nicotine replacement therapy)
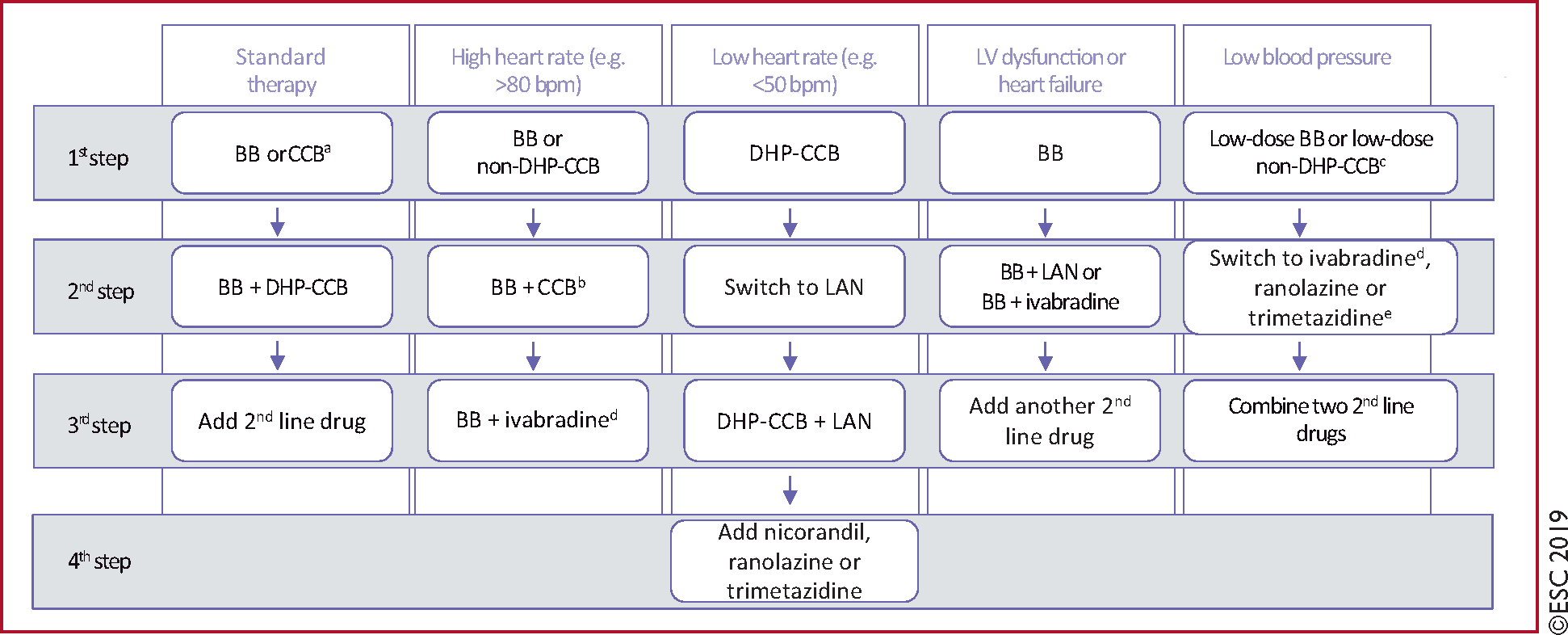
- Beta blockers (first line if rEF or history of MI) targeting heart rate 55-50
- Beta blockers or long acting CCB in uncomplicated patients (don’t combine non-dihydropyridine CCB with Beta blockers)
- Long acting nitrate (in addition to above if still symptomatic)
- Third line medications: ivabradine (only one available in Canada), nicorandil, ranolazine, and trimetazidine
Invasive Coronary Angiography
Referral for Invasive Testing/Cath (CCS)
| 1. We recommend that coronary angiography be considered early in patients who are identified to have high-risk non-invasive test features (Strong Recommendation, High-Quality Evidence). |
| 2. We recommend that patients who develop medically refractory symptoms or inadequate CV quality of life while using medical therapy should undergo elective coronary angiography in anticipation of possible revascularization procedures (Strong Recommendation, High-Quality Evidence). |
- Note: goal of invasive coronary angiography for high risk patients is to identify anatomy where revascularization has a prognostic benefit (ie. diabetes and multivessel disease)
Revascularization Considerations
- Evolving story with new evidence coming out (ie. ISCHEMIA trial)
- Two main indications for revascularization:
- Refractory symptoms despite medical management
- Anatomy with proven prognostic benefit for revascularization
- Consider CABG:
- Left Main Disease >50% (debated PCI vs CABG)
- Multivessel disease* and diabetes
- Mutlivessel disease* with LV dysfunction
- If CABG not an option, can consider PCI
- Note this framework is for stable CAD as acute coronary syndrome is approached differently
*Multivessel disease defined as ≥70% stenosis in ≥2 major epicardial vessels and ≥2 separate territories
Further Reading
Authors
- Primary Author: Dr. Atul Jaidka (MD, FRCPC, Cardiology Fellow)
- Author/Reviewer: Dr. Pavel Antiperovitch (MD, FRCPC, Cardiology Fellow)
- Staff Reviewer: Dr. Michael Ward (MD, FRCPC[Cardiology])
- Copy Editor: Perri Deacon (medical student)
- Last Updated: March 25, 2020
- Comments or questions please email feedback@cardioguide.ca