Abbreviations
- SCAD – Spontaneous Coronary Artery Dissection
- CAD – Coronary Artery disease
- MINOCA – Myocardial Injury with Non-Obstructive Coronary Artery Disease
- ACS – Acute Coronary Syndrome
- AMI – Acute Myocardial Infarction (MI)
- OCT – Optical Coherence Tomography
- IVUS – Intravascular ultrasound
- FMD – Fibromuscular Dysplasia
Spontaneous Coronary Artery Dissection (SCAD)
- Non-atherosclerotic non-traumatic cause of acute coronary syndrome and death
- 4% of all ACS
- 35% of ACS in woman < 50yo.
- High level evidence to direct management is not available
- Pathophysiology
- Development of hematoma within tunica media of vessel, leading to separation of intima from media (see figure).
- This compresses the true lumen causing ischemia and AMI.
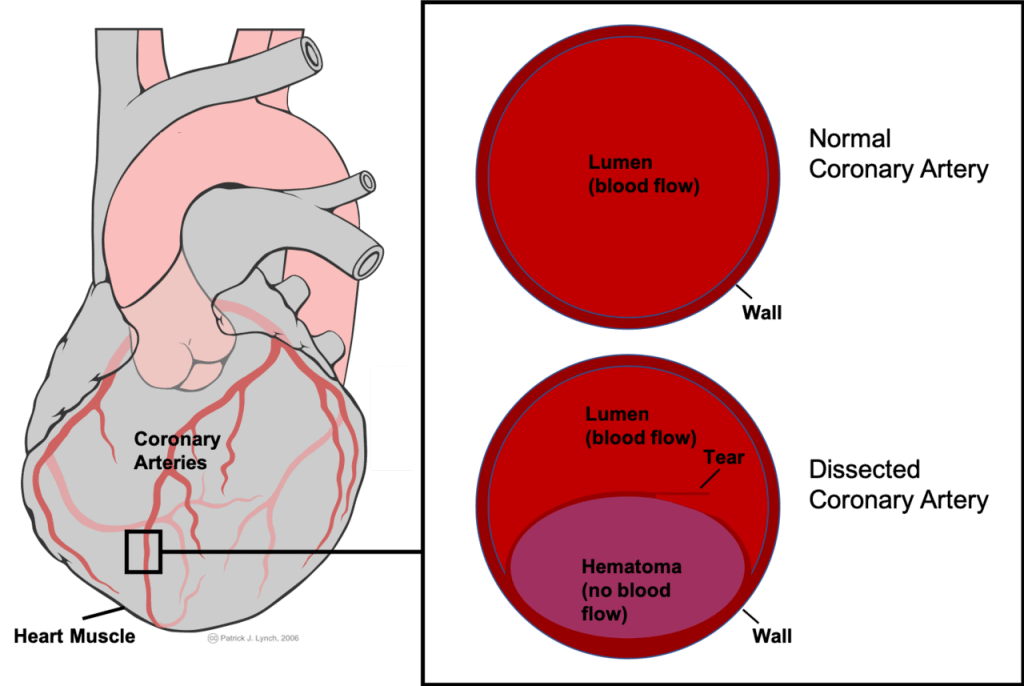
- Two hypotheses:
- “Inside-out” – blood enters the subintimal space from true lumen after endothelial-intimal disruption “flap”.
- “Outside-in” – hematoma arises de novo in the media, possibly from microvessels.
- Three types:
- Type 1 – Multiple radiolucent lumens with arterial wall staining
- Type 2 – Diffuse stenosis
- Type 3 – focal tubular stenosis mimicking atherosclerosis
- Risk Factors
- Multifactorial **
- Hormones
- Sex
- Genetics (connective tissue diseases)
- Pregnancy (70% within 1st week postpartum) – termed P-SCAD, more severe
- Emotional stressors more common triggers in women.
- Physical stressors more common in men (cocaine, retching, cancer)
- Multifactorial **
- Presentation
- Classically middle-aged women without significant CAD risk factors.
- Present as overall ACS (STEMI or NSTEMI) syndrome.
- Chest pain, Troponin rise, ECG findings (ST elevations or depressions)
- Ventricular arrhythmias, shock, arrest.
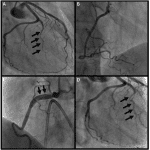
- Diagnosis
- Coronary Angiography
- Usually mid-to-distal coronary artery (typically LAD)
- Intracoronary imaging can help confirm diagnosis (OCT and intravascular ultrasound (IVUS))
- Usually not done unless diagnosis uncertain – instrumenting vessels can cause injury.
- CTA may identify large-vessel SCAD, but lacks spacial resolution.
- Coronary Angiography
Management
- Generally presents similar to acute MI, angiography needed to diagnose.
- If pregnant –> fetal shielding
- Most patients recover normal coronary architecture within 30 days (95%)
- 10-30% lifetime recurrence
- Interventional Management
- PCI results are unpredictable, high risk of complications, suboptimal outcomes.
- Can worsen dissection and cause complete occlusion. (1/3 have hematoma propagation)
- Resorption of hematoma can cause poor stent sizing/malapposition
- Generally treated as conservatively as possible.
- Stenting/CABG can be considered for large vessel high-risk dissections (left-main, shock, pain)
- PCI results are unpredictable, high risk of complications, suboptimal outcomes.
- Pharmacologic Management
- Treat any LV dysfunction with standard HF therapy
- Beta-blocker (lower rates of recurrence in some studies)
- Lipid management – only if indication
- ASA / DAPT – No specific recommendations. Most clinicians recommend DAPT for 2-4 weeks then ASA for 3-12 months. (skip if high risk of bleeding)
- Anti-angina pain management (nitrates, analgesics)
- Non-Pharmacologic
- Strong relationship to fibromuscular dysplasia (FMD)
- Many consensus papers recommend FMD (arteriopathy) screen head to pelvis with CTA or MRA.
- May identify clinically important vascular complications that may warrant treatment/follow-up (such as intracranial aneurysm)
- Avoid high-intensity/extreme-endurance/competitive aerobic and isometric exercise (tends to trigger (SCAD))
- Moderate intensity exercise is encouraged – benefit likely outweighs the theoretical risk of recurrent SCAD
- Avoid heavy lifting that require prolonged straining/valsalva
- Strong relationship to fibromuscular dysplasia (FMD)
References
- JACC – State of the art Reviews
Authors
- Primary Author: Pavel Antiperovitch (MD, FRCPC Cardiologist)
- Reviewer: TBD
- Copy Editor: TBD