Introduction
- Please see original article: Syncope for full details on the differential and diagnostic approach to syncope
- Details regarding pacing will be discussed in other topics, a general overview of indications for pacing in patients with cardiac syncope will be outlined below.
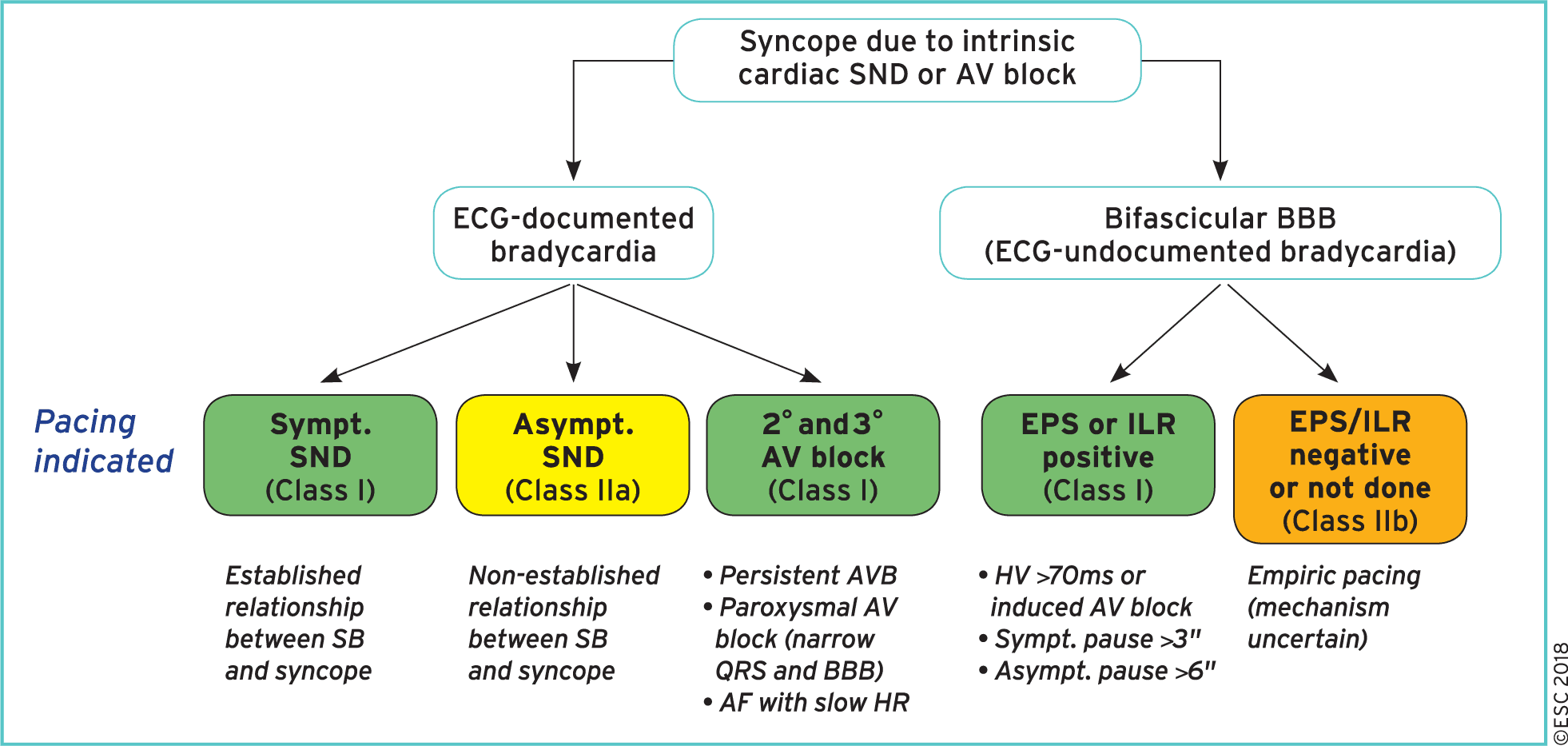
Bradycardia related syncope
- Cardiac pacing is indicated when there is an established relationship between syncope and symptomatic bradycardia due to (Class I):
- Sick sinus syndrome
- Intrinsic AV block
- Cardiac pacing is indicated in intermittent/paroxysmal intrinsic third- or second-degree AV block (including AF with slow ventricular conduction), although there is no documentation of a correlation between symptoms and ECGs (Class I).
- Cardiac pacing should be considered when the relationship between syncope and asymptomatic sinus node dysfunction is less established (Class IIa)
Bifascicular Bundle Branch Block
- Pacing indicated in patient with syncope, bundle branch block and documented AV block AV block on loop recorder or positive electrophysiology study (Class I)
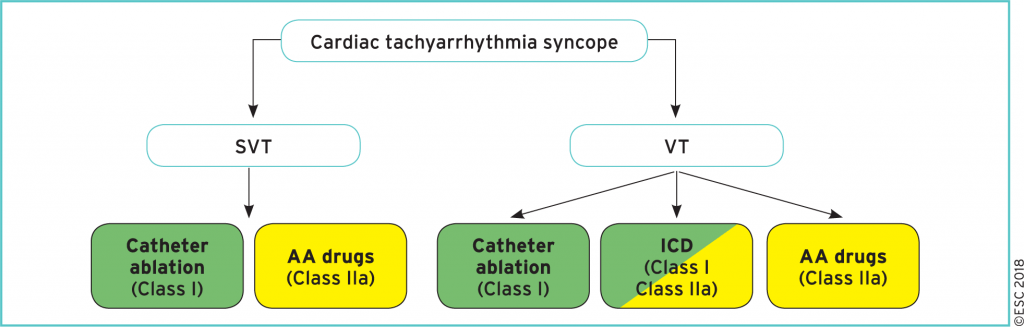
Tachycardia related syncope
- Catheter ablation is indicated in patients with syncope due to SVT or VT in order to prevent syncope recurrence. (Class I)
- An ICD is indicated in patients with syncope due to VT and an ejection fraction <35% (Class I)
- An ICD is indicated in patients with syncope and previous myocardial infarction who have VT induced during EPS (Class I)
- An ICD should be considered in patients with an ejection fraction >35% with recurrent syncope due to VT when catheter ablation and pharmacological therapy have failed or could not be performed. (Class IIa)
- Antiarrhythmic drug therapy, including rate-control drugs, should be considered in patients with syncope due to SVT or VT. (Class IIa)
Structural Causes
- Syncope in patients with structural heart disease or inheritable arrhythmia syndromes is associated with a two- to four-fold increased risk of death!
- Implantable cardioverter defibrillator indications in patients with unexplained syncope and left ventricular systolic dysfunction:
- ICD therapy is recommended to reduce SCD in patients with symptomatic heart failure (NYHA class II–III) and LVEF <35% after >3 months of optimal medical therapy, who are expected to survive >1 year with good functional status.(Class I)
- ICD should be considered in patients with unexplained syncope with systolic impairment, but without a current indication for ICD, to reduce the risk of sudden death (Class IIa)
- Implantable loop recorder (instead of ICD) may be considered in patients with recurrent episodes of unexplained syncope with systolic impairment, but without a current indication for ICD. (Class IIb)
- Topics of Hypertrophic cardiomyopathy, Arrhythmogenic right ventricular cardiomyopathy, Long QT syndrome will be discussed separately.
Further Reading
Authors
- Primary Author: Dr. Dimitar Saveski (MD, FRCPC, Internal Medicine Resident)
- Author/Reviewer: pending (MD, FRCPC, Cardiology Fellow)
- Staff Reviewer: pending (MD, FRCPC[Cardiology])
- Last Updated: April 7, 2020
- Comments or questions please email feedback@cardioguide.ca